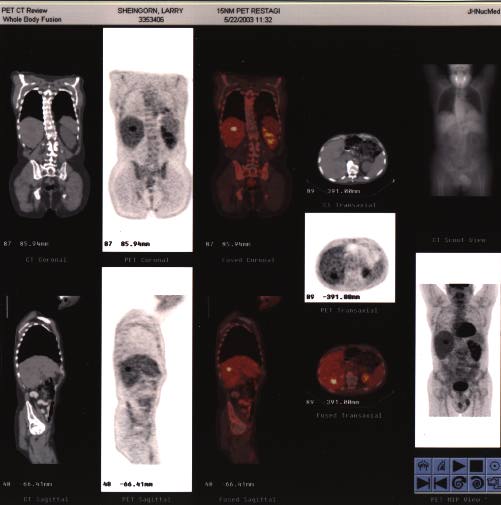
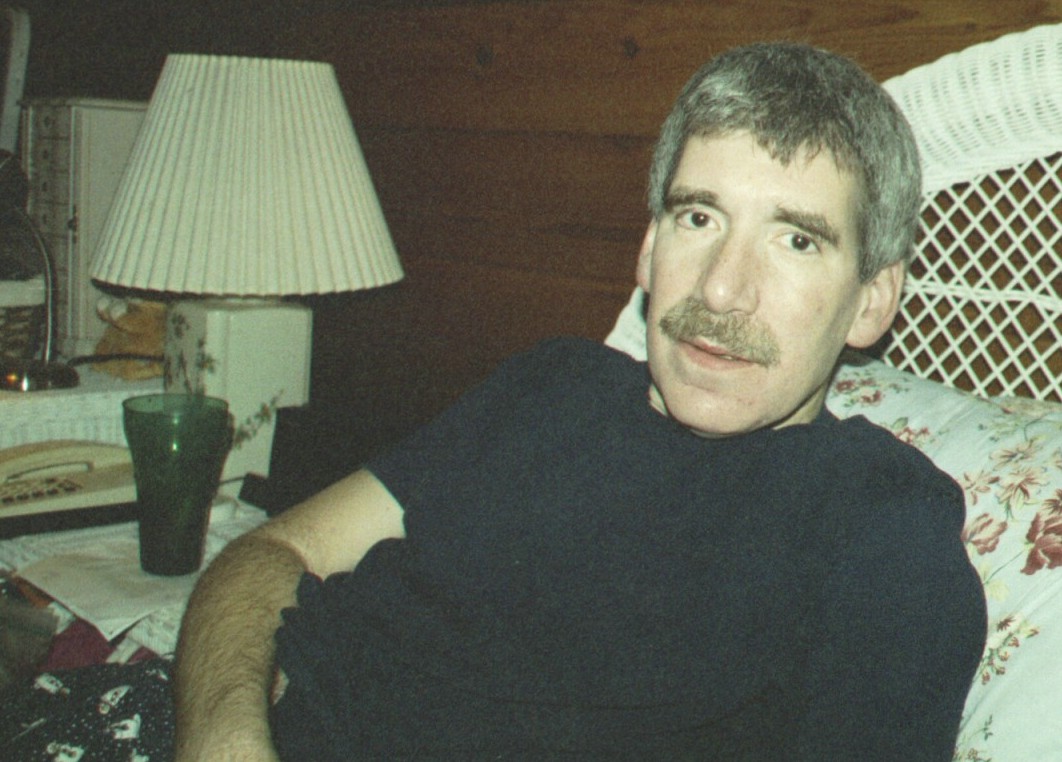
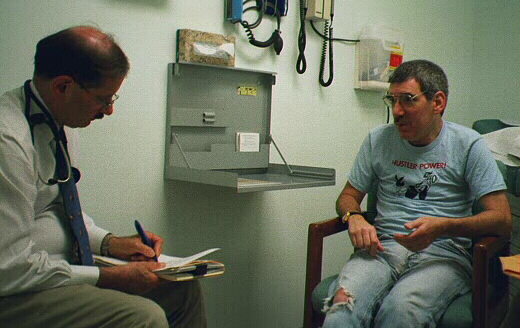
dx'd: 02/15/01 via routine endoscopy
 |
The lesion measured about 2 x 4 cm, and was essentially asymptomatic. |
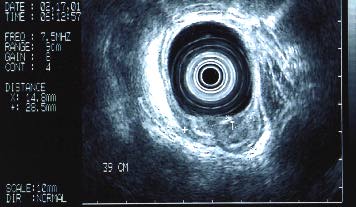
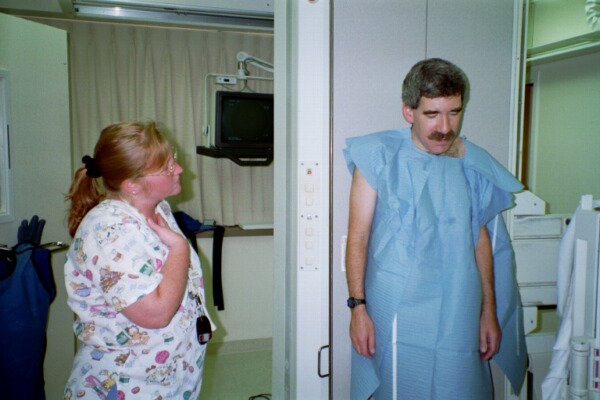
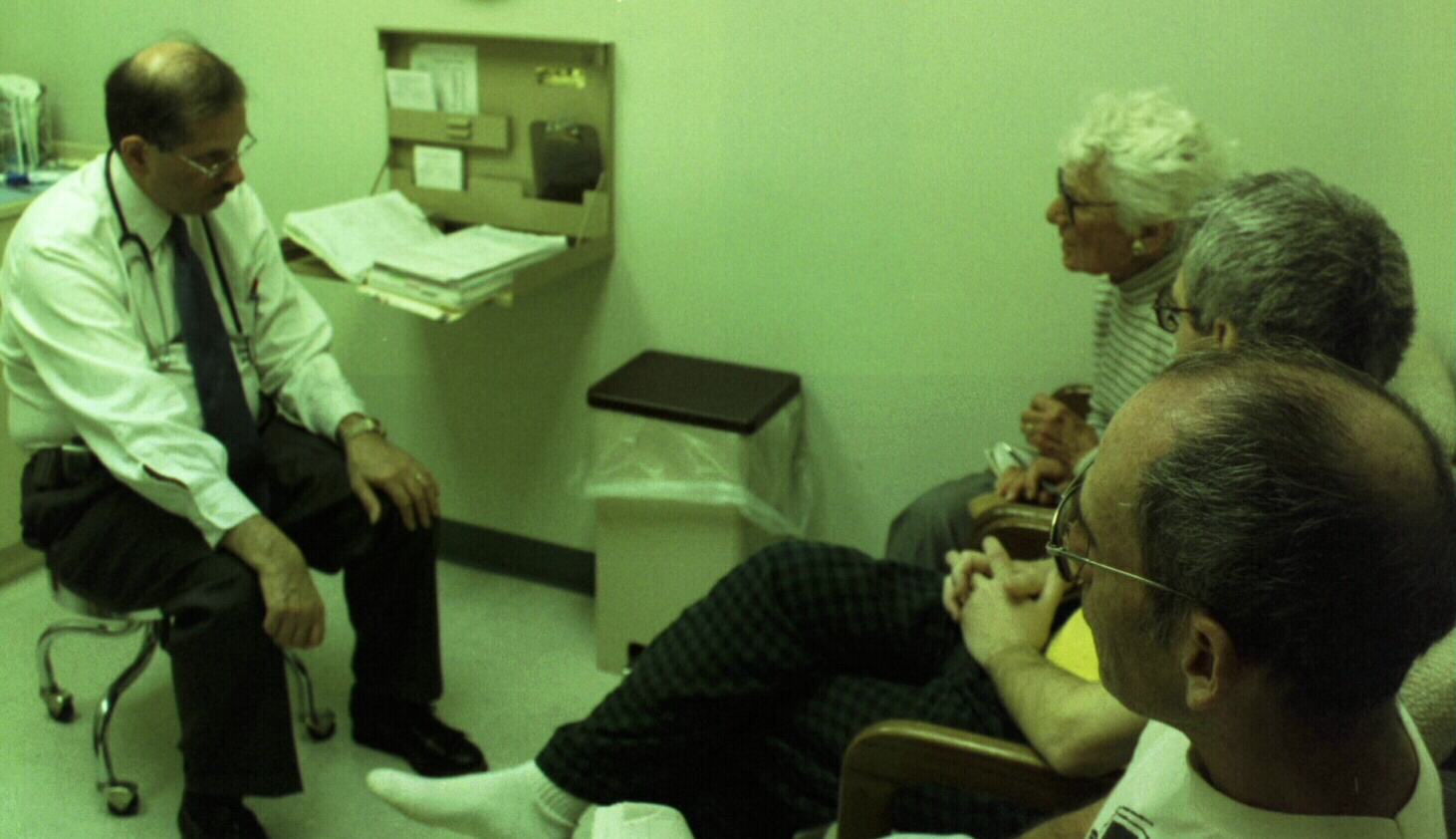
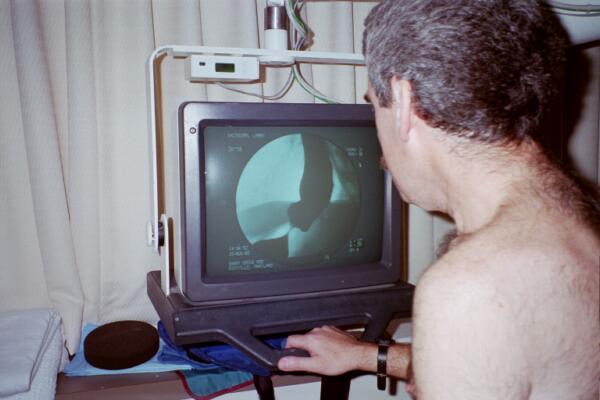
02/16/01: esophageal ultrasound
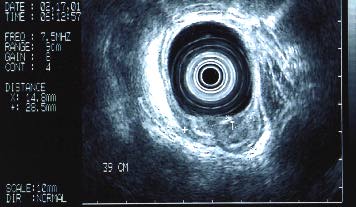 |
stage T2-N1-Mx so far |
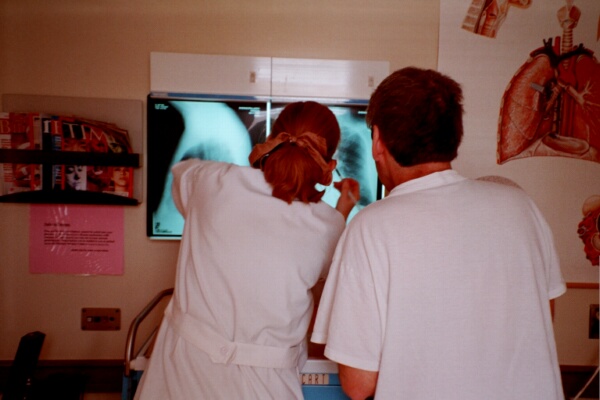
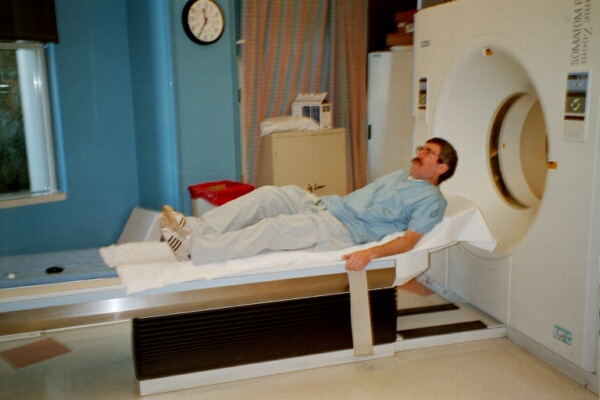
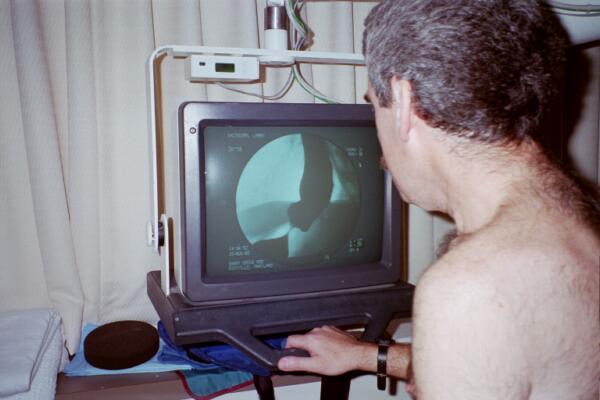
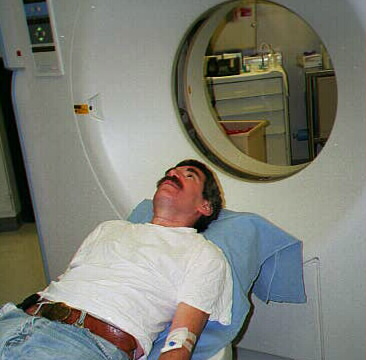
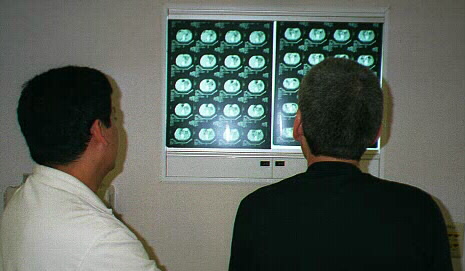
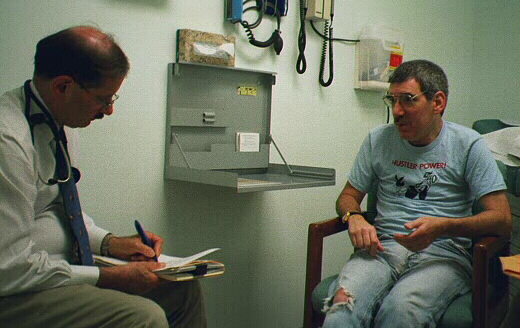
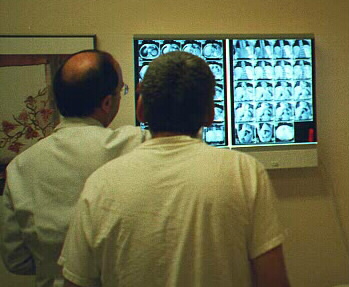
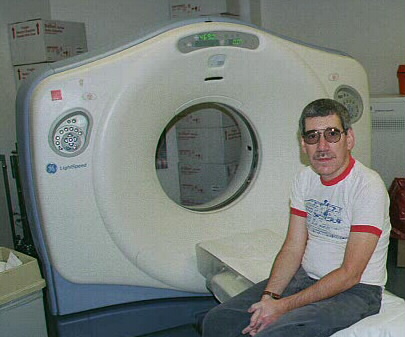
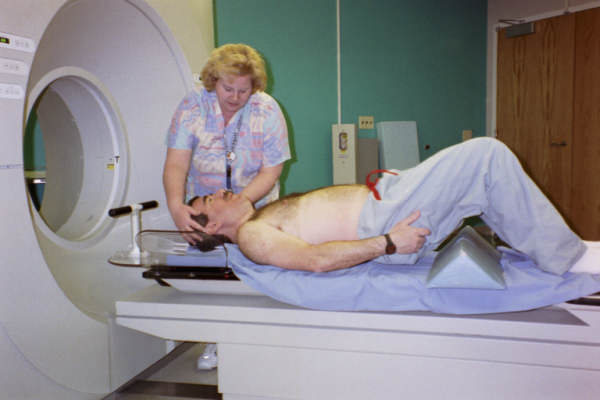
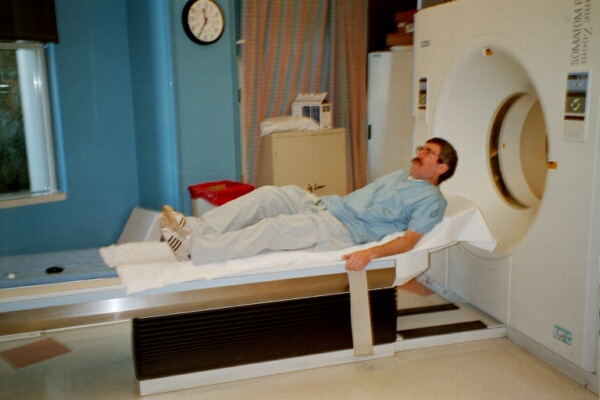
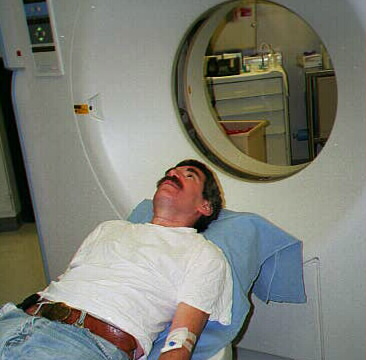
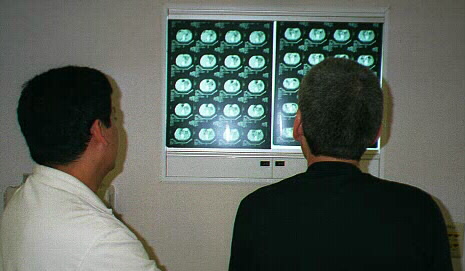
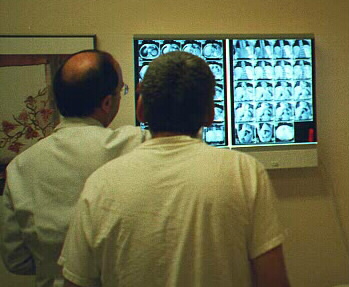
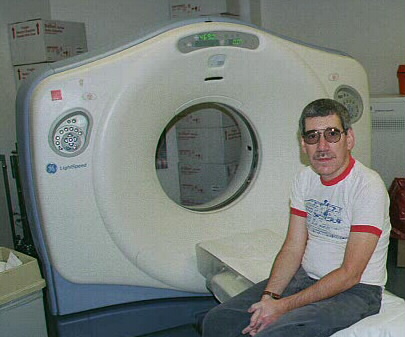
02/17/01: CAT scan
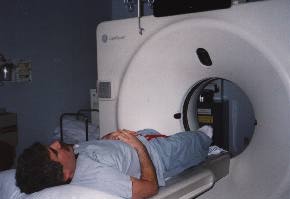 |
 |
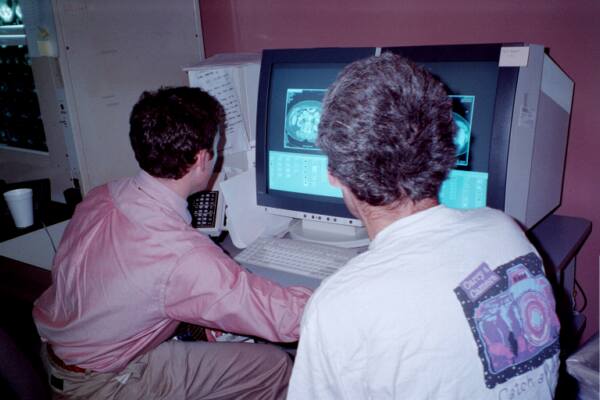
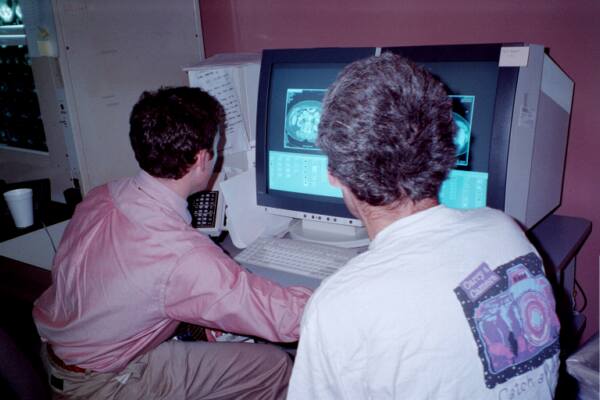
An advantage of being an MD -- you can look at your own scan.
Thankfully, showed no mets! |
| TRIPS TO SEE THE EXPERTS |
|
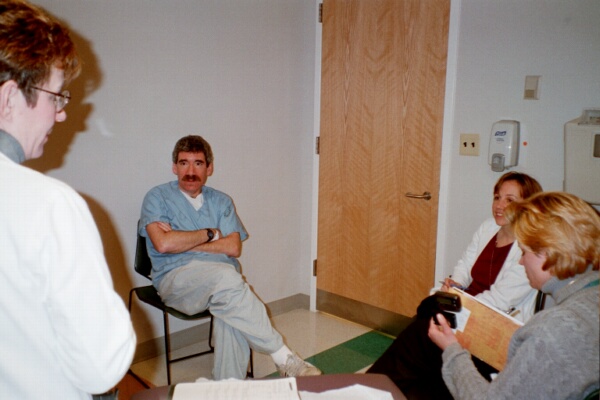
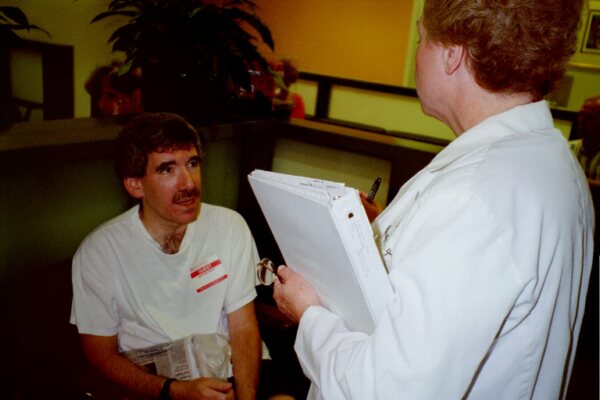
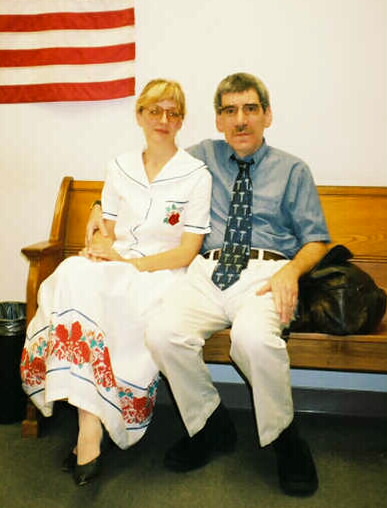
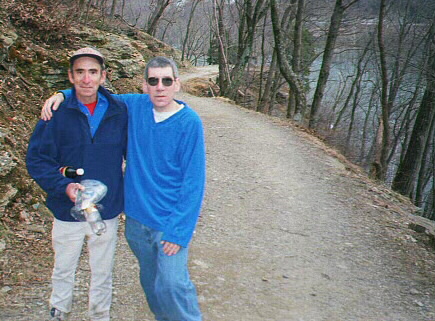
02/21/01: Sloan-Kettering (note the haircut in anticipation of surgery)
 |
Valerie Rusch -- suggested an esophagectomy without chemo/rad, and feels I
have a 40% chance of living 5 years.
 |
The plane ride home was one of the most depressing times I can remember.
|
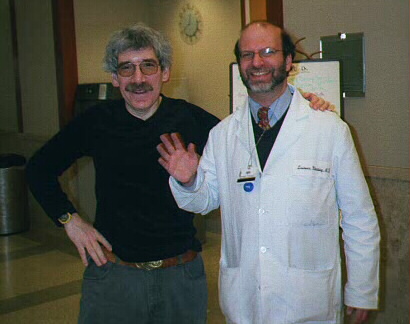
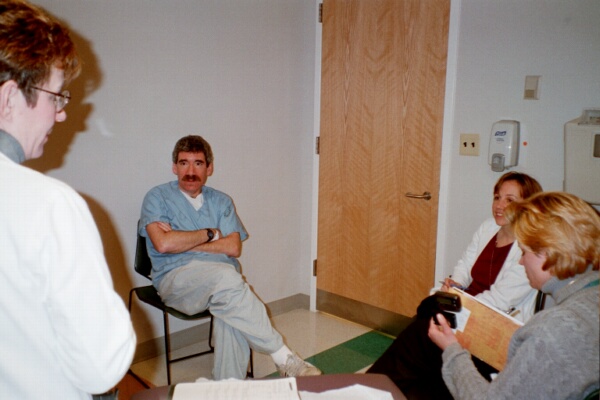
02/23/01: David Sugarbaker/Brigham and Women's Hospital
 |
His opinion: "you only have one shot at this, so hit it hard". He suggests
aggressive chemo/rad, followed by radical esophagectomy, followed by more
chemo. I liked his approach -- while other doctors and institutions looked at me
as if I was already dead, Dr. Sugarbaker's enthusiam gave me hope. And something
about his office staff and environment gave me a good feeling, too. (12/01: I was half-right!
Be sure to see the note about the office below.) |
02/27/01 AM: Arlene Forastiere/Johns Hopkins
 |
Although having her manage my chemo/rad means I have to move to Baltimore for
many months, the more I interact with her and her staff, the more I trust
their oncology skills. |
 |
02/27/01 PM: Dan Haller/University of Pennsylvania
 |
He gave me a pedantic lecture, using abbreviations he did not define and
which I did not understand (and I'm a physician!), and spent much of
our time complaining about his colleagues stealing his research topics and
beating him to publication. I'm sure he is a brilliant statistician and
oncologist, but, in my mind, he should not be seeing patients. At least not
me. His associate's advice: "take a vacation . . . (before you die)". |
02/27/01 PM: Ernest Rosato/University of Pennsylvania
 |
Told me I had a tough problem, that I've seen the experts, and there is no
one "right" way to handle this. His advice: "You've intellectualized enough.
Probably too much. Its time to get off the dime." A warm, genuine guy, who I
would let operate on me any time. He put himself at my service if I so
desired, and I remain grateful. |
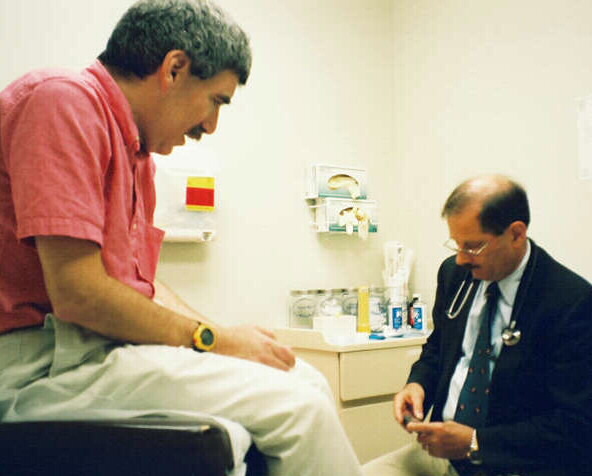
03/06/01: Fred Smith
 |
He cared for my mother's breast cancer, and I visited him for one more
opinion. He agreed I have a bad disease, but assured me I was in the best of
hands. He offered to be there any time. Another competent, compassionate,
physician who is helping me through this difficult time. |
| * * MY PLAN * *
|
 chemo by Forastiere
chemo by Forastiere
|
surgery by Sugarbaker

|
| * * * * * * * |
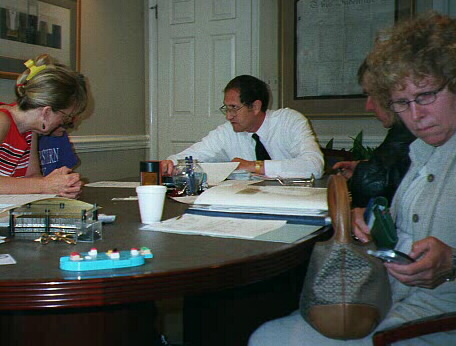
| STAGING AT HOPKINS/TREATMENT PREP |
03/02/01: injection for PET scan. Doctors make the worst patients.

They tell you to sit absolutely still for 45 minutes after the injection. I
haven't sat still for 45 minutes since I was born! |
PET scan

|
Thankfully, scan showed no mets

|
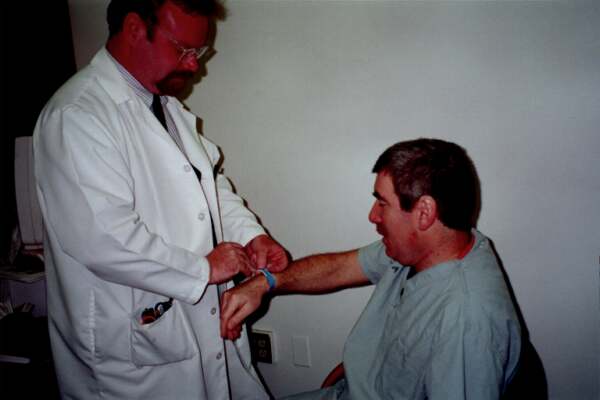
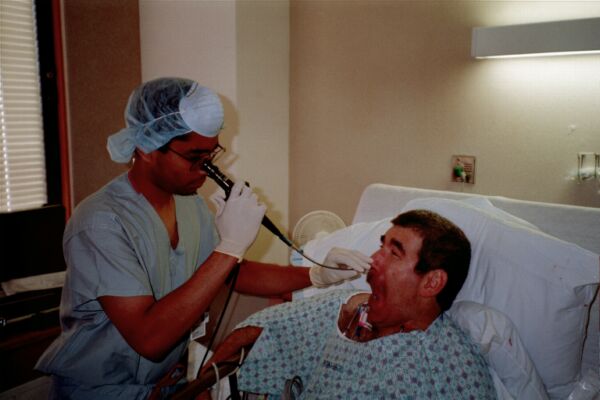
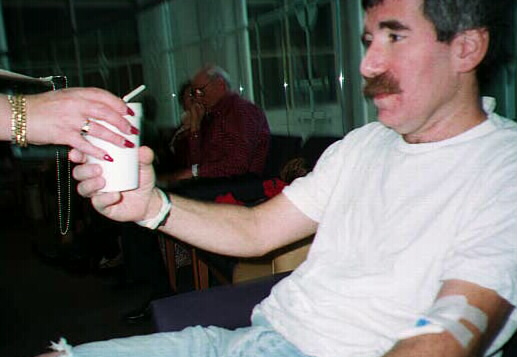
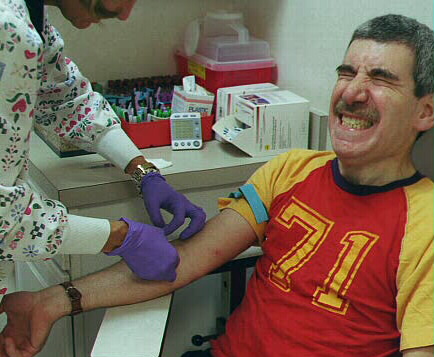
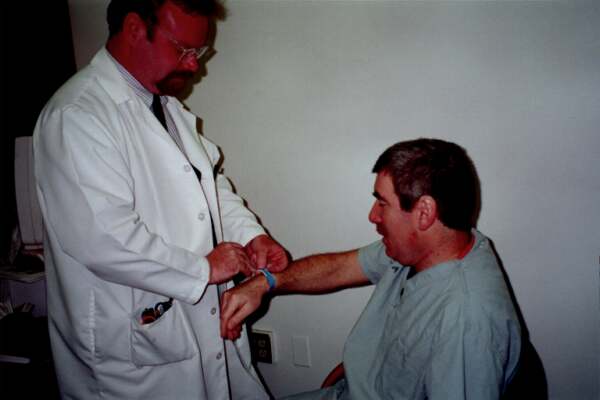
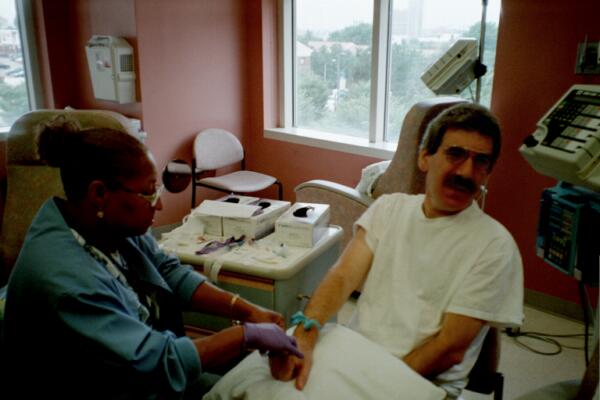
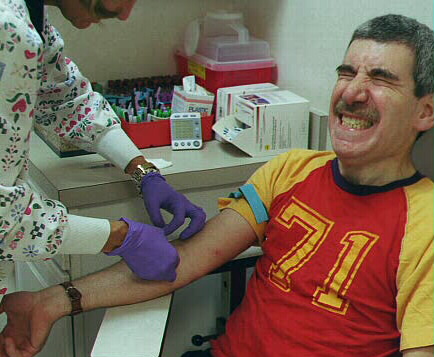
03/07/01:

|
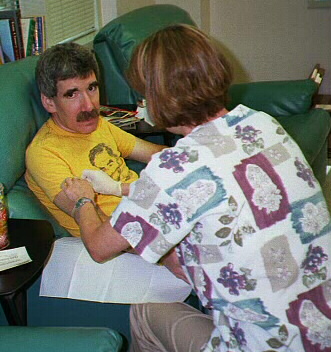
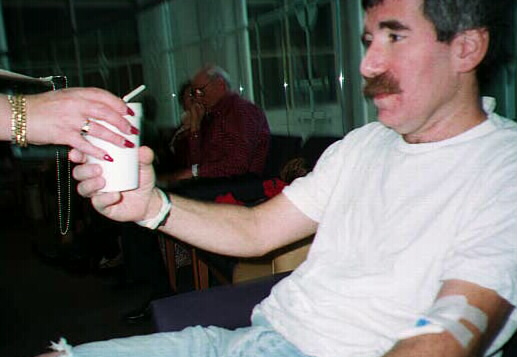
Another in a seemingly endless stream of needlesticks. This time, for a
repeat endoscopy. Findings were essentially unchanged, and the hope is I
don't have metastatic disease. |
|

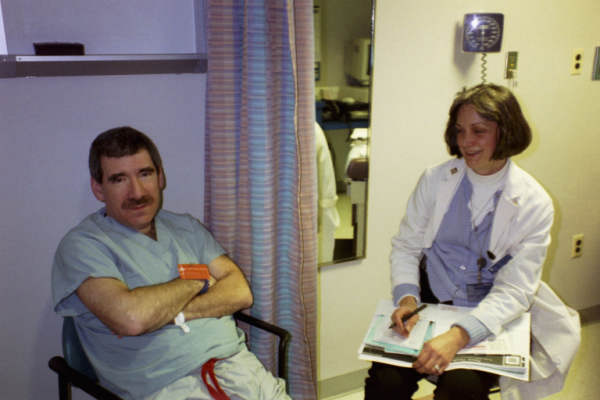
|
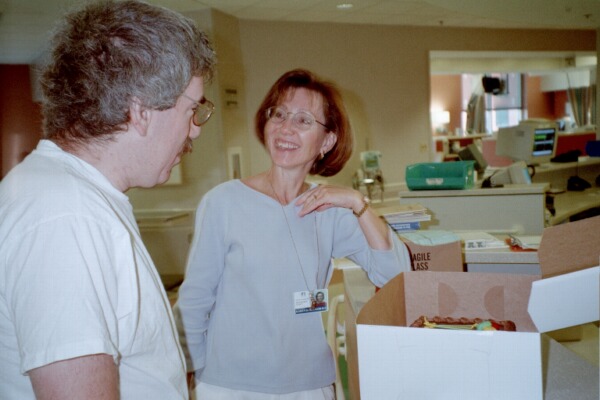
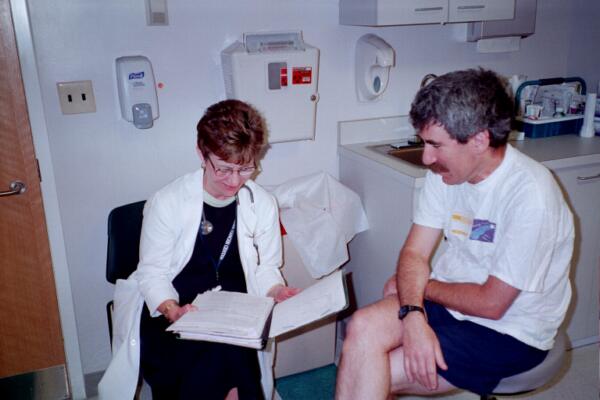
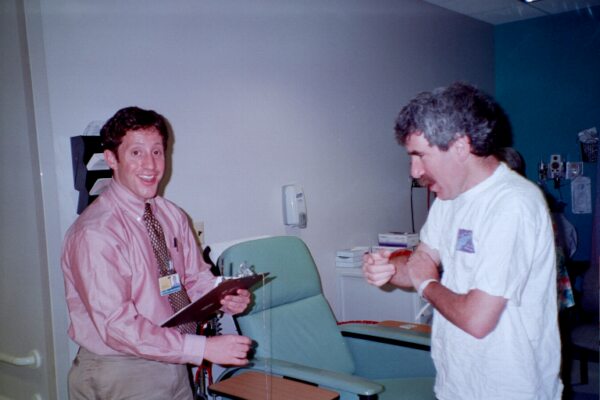
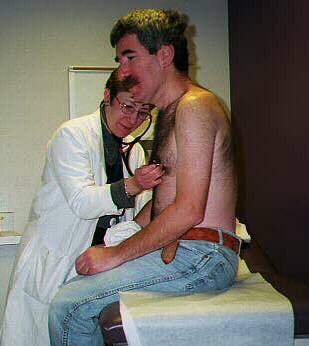
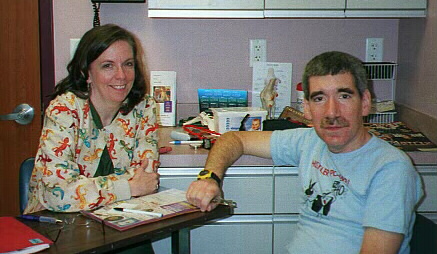
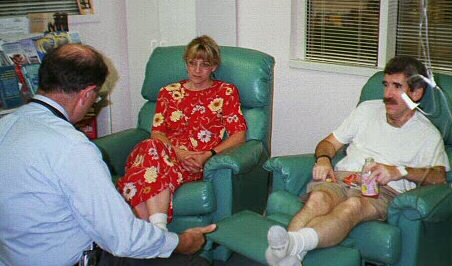
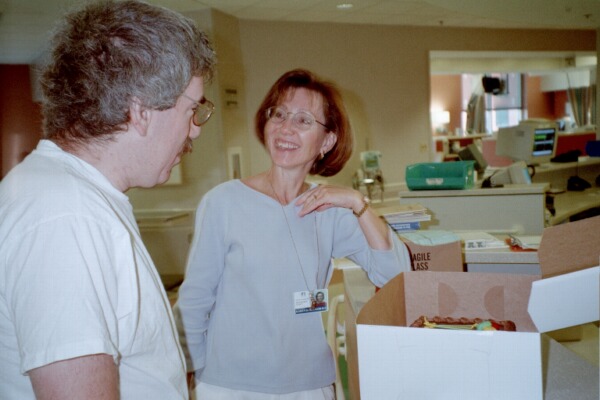
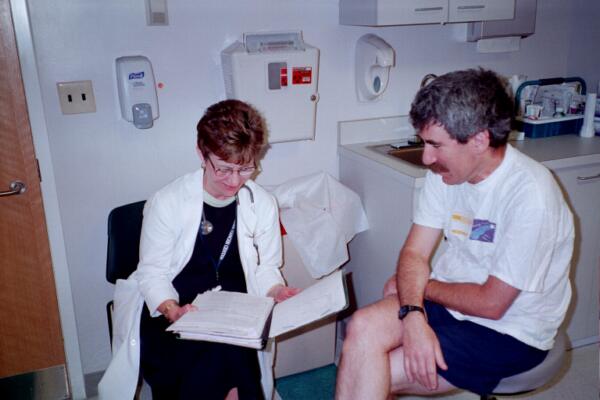
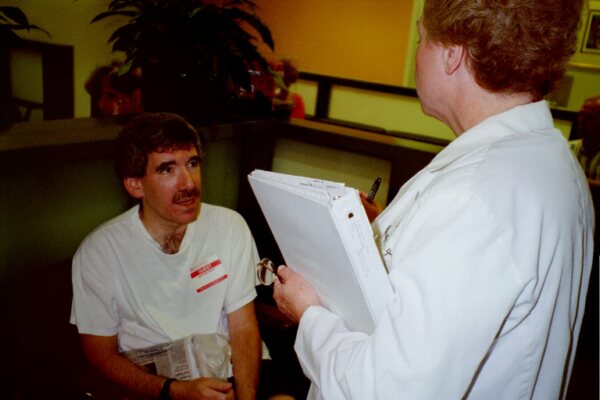
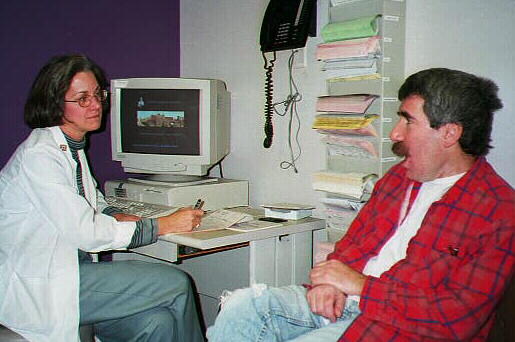
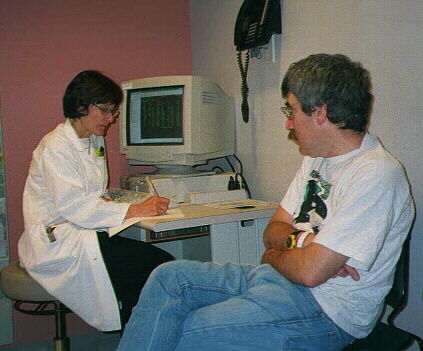
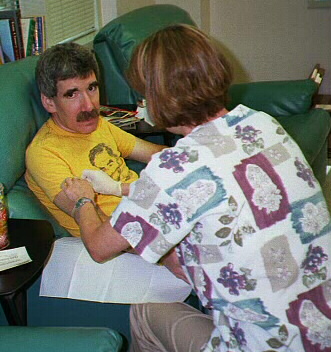
Arlene telling me to keep a positive attitude. She is optimistic after
reviewing latest EUS.
|
|
|
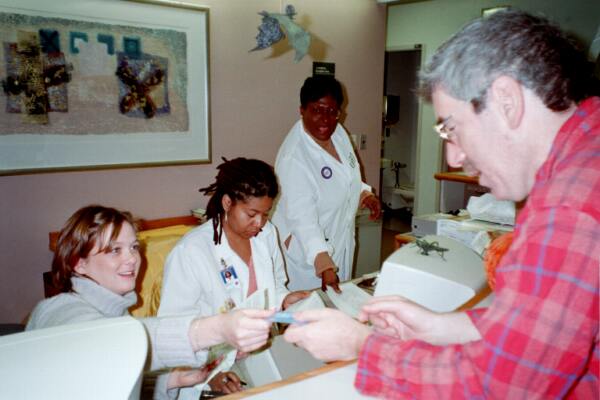
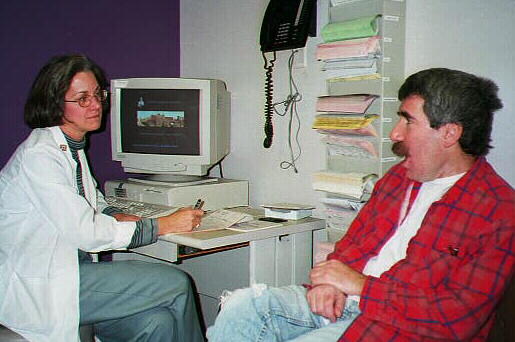
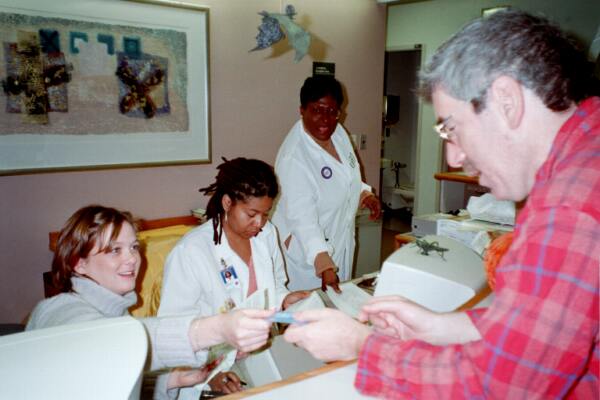
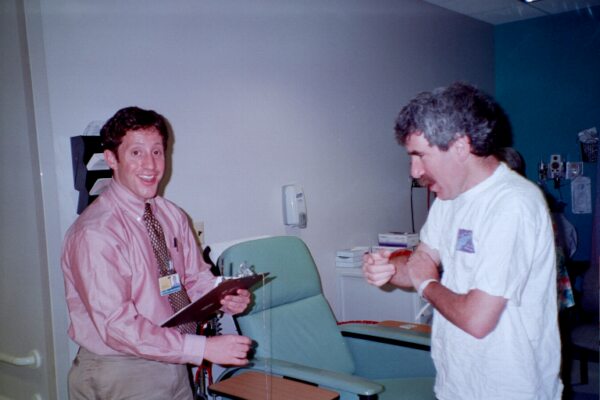
Keeping track of all the appointments, procedures, etc., in a strange
city, no less, is overwhelming. Nurse coordinators help. Here, Nancy Tsottles
answers a question, undoubtedly for at least the third time! |
03/09/01:

|
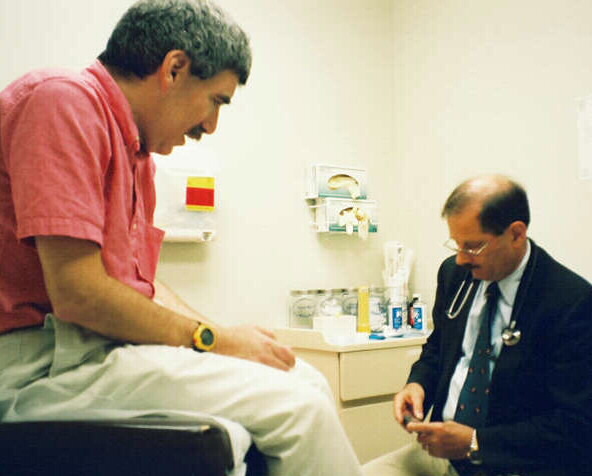
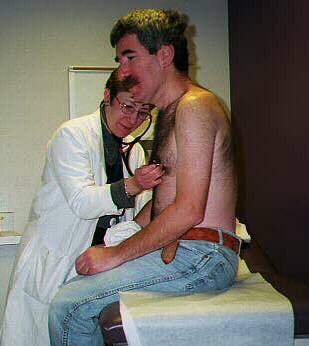
Meeting the radiation oncologist (Dr. Kleinberg) and his staff. Again, he
couldn't be nicer! Now if only he didn't have to zap my esophagus . . . |
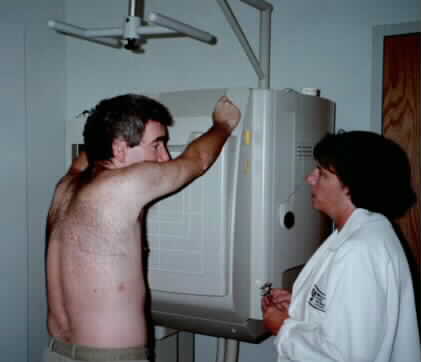
03/09/01: radiation "SIM"
|
Another CAT scan, and the first of many marks on my chest, allows them to
accurately aim the radiation treatments during the coming month. Nothing
hurts except my pride. |
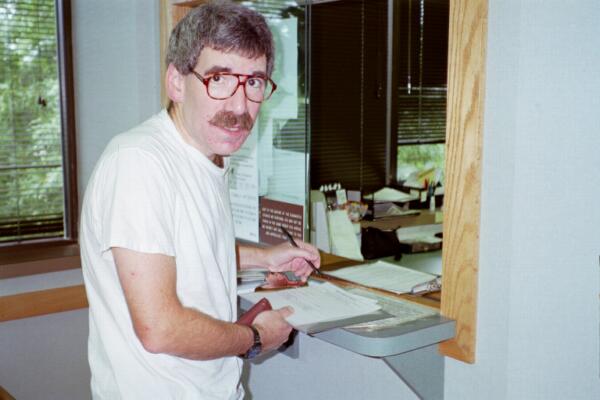
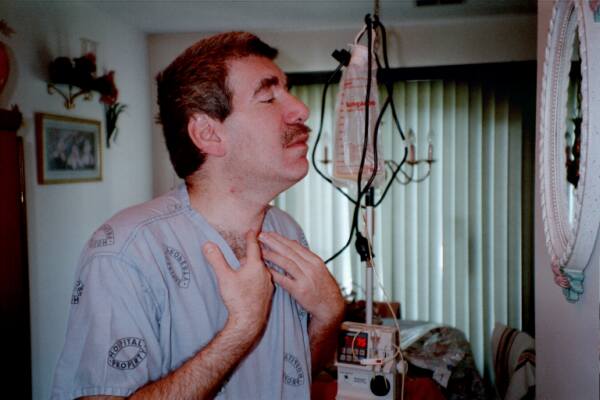
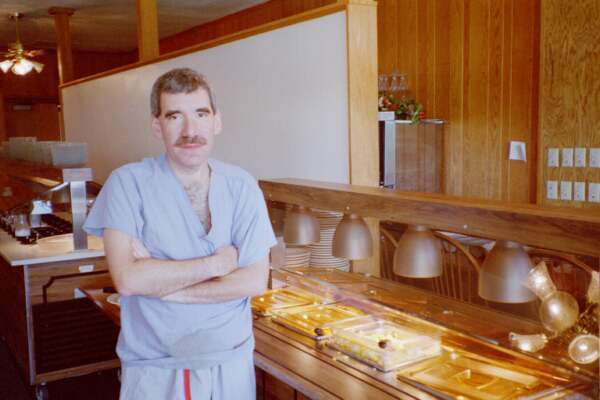
03/12/01: A strange feeling, coming to my own hospital for implantation of a
Hickman catheter!
 |
Definitely among friends . . . the SAME desk where I wait for my cataract
patients . . . .

|
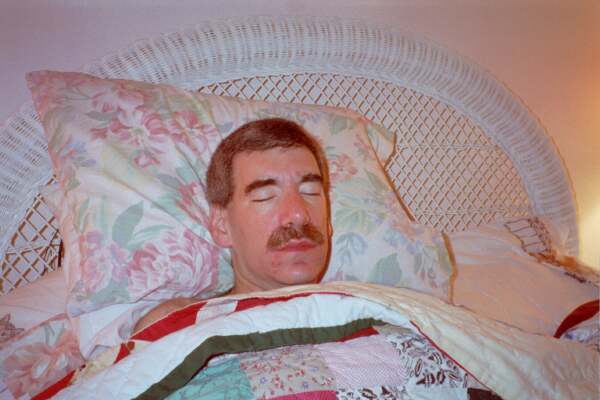
When I awake, I'll have a tube sticking out of my chest. Depressing . . . .

|
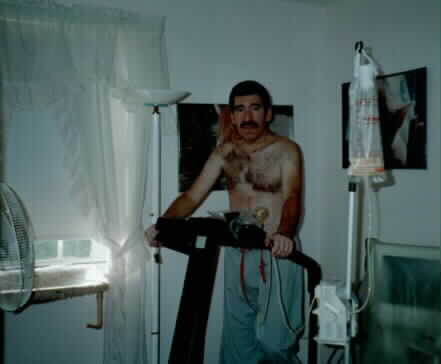
| J9979 Treatment - start 03/15/01 |
|

|
They tell you the pump is "like a Gameboy", but after having it attached to
you day and night, it's a pain! Every few minutes, it pumps a
chemotheraputic agent - 5FU - through the Hickman. A counter starts at 96,
and just as I feel a sense of relief that its down to 12, its time to
reload! The 5FU makes me tired, and slightly nauseous, I think, but they
tell me I'm "tolerating it well". |
 |
 |
Monday through Friday I have radiation. You lie on a table, and they go over
marks with "indelible" ink. I can't shake the feeling they are doodling
(especially when they yell "YATZEE"). The treatment itself only takes 15
seconds or so. Sometimes the hair all over my chest "stands up" during the
treatment, and they've never been able to explain it.
I don't enjoy this at all, even the waiting room makes me nauseous -- its
muggy -- but maybe EVERYTHING makes me nauseous now! |

|
 |
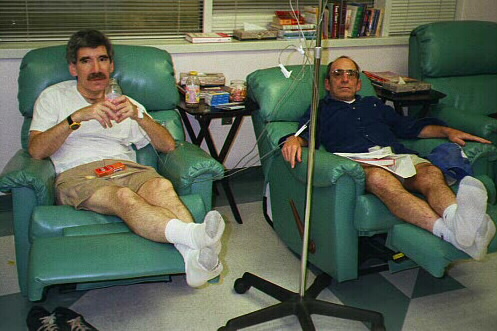
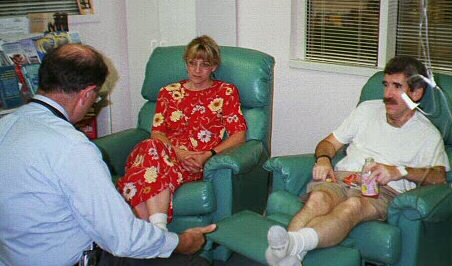
For 2, 5 day runs, they give you CISPLATIN, another chemo agent. This is
given over an hour or so, after an hour or so of hydration. It makes me
feel worse than the 5FU, I think, but because of IV meds, I only vomited
once. And that kind of snuck up on me! I think the trick might be to try
to take anti-nausea meds BEFORE you feel very sick.
My appetite is zero, but they tell me if I lose too much weight, they'll
feed me with a tube, so I eat! Curiously, eating does not seem to make the
nausea much worse. |
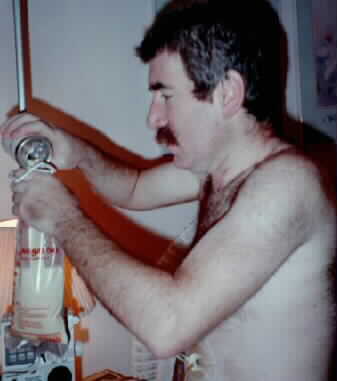
 |
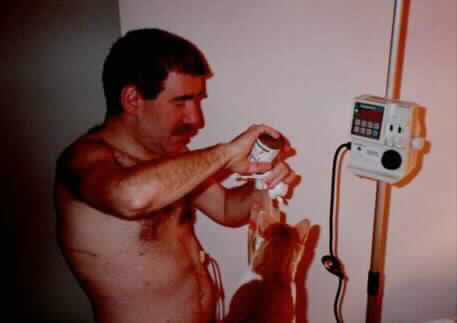
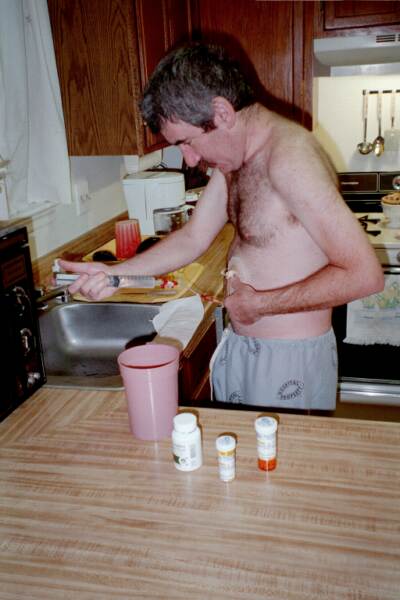
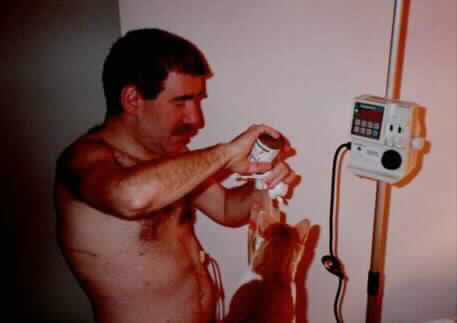
Recently, using a medicine container, a drill, and a Dremmel tool, I made a
better cathater holder than the chain and adhesive tape! Still, I miss
relaxing and thinking in the shower. Now, I have to dance around the tubing,
and spend 30 minutes afterwards attending to the Hickman dressing. All the
while feeling sick.
If all this allows me to live a normal life, it will be worth it; if not,
what a bummer! |
 |
|
03/30/01:
 |
Can you believe it? For reasons that are still not 100% clear (and the
usual suspects aren't talking), the Hickman catheter implanted on 3/12/01
was expired. In and of itself, I don't think that was clinically
significant, but its position was apparently poor, requiring me to stand
on my head to get blood. It was replaced on 3/30/01. |
|


|
During the chemo/radiation treatments, there were times I felt so
sick I had to force myself to eat, remembering the threat of a "J tube"
(for feeding). My own mother's matzoball soup didn't help. The Zofran,
Compazine, and Atavan, I suppose, helped, but I felt like I was hit over
the head with a frying pan. I suggested I try Marinol (the "marijuana pill"),
but the oncologists assured me this wouldn't help. Finally on 4/19/01, I
told one of the nurses I was SO miserable I couldn't eat, drink, sleep, or
think, and she said, off the record, why not take the Marinol? Within 2
hours -- for the first time in at least a month -- I walked to the Inner
Harbor and ate a hot dog, without gagging, with my mother.
I have no idea why my doctors were so reluctant to suggest Marinol, (the
usual suspects -- different ones this time -- are not talking), but for me
it was a God-send. Moral to physicians: listen to your patients! If
they tell you they feel terrible, at least offer to let them try this class
III drug. Moral to patients: if you are suffering, try the drug or know the
reason why. |
 |
After 3 months of chemo and radiation, tests continued to give an optimistic
picture of no metastases. All the doctors and nurses at Hopkins wish me well,
and if I live, they get much of the credit, but I wish I could have met
them under different circumstances! |
 |
 |
06/23/01: Just a week before my surgery, I developed shaking chills, and a
temperature of 105! I had to be admitted to Shady Grove Hospital, again.
Cultures showed a gram negative bacteremia. Antibiotics and removal of the
second Hickman catheter gave me improvement. |
 |
 |
I'll remember the month before the esophagectomy as one mainly of fatigue,
milder discomfort, nausea, and fear. I realize how much I enjoy life, and
how very much I want to continue my activities as before. And, yes, the
Epogin shots, once/week, do sting like hell. |
 |
|
May 27, 2001: I go to Boston next week for an esophagectomy on the 31st, at
9:00 AM. I am scared, but think my doctors are probably among the most
skilled in the world in this field. I am optimistic I will do well. Wish me
luck!!! |
| SURGERY IN BOSTON |
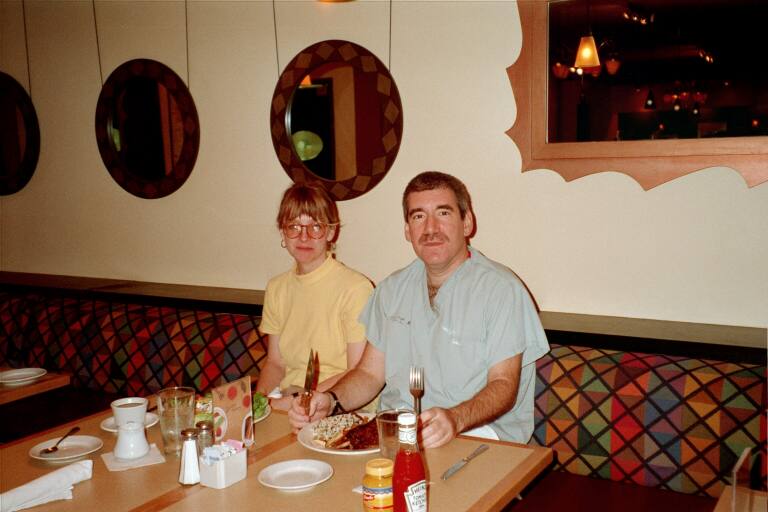 |
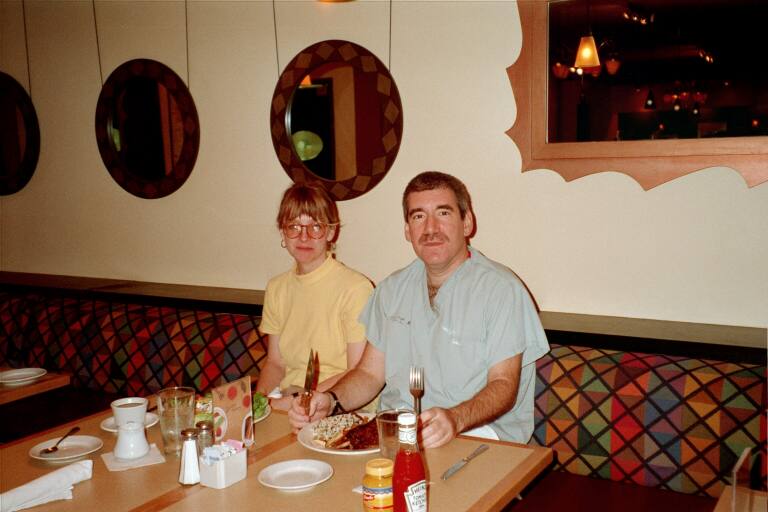
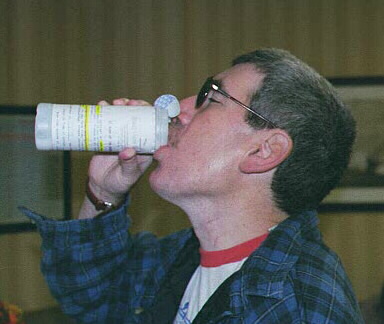
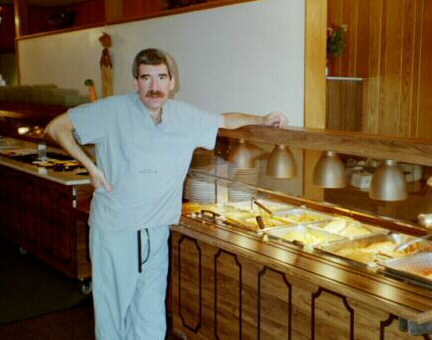
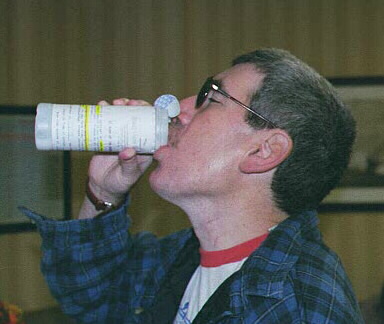
Although everyone is optimistic I will lead a normal life after the surgery,
they tell me I might never eat the same again. For my last meal, 48 hours
pre-op, I had steak and fries.
Actually, it turns out my real last meal was a bottle of "GoLytely"
and antibiotics, used as a surgical prep. I didn't realize how good a glass
of water would taste to me a week later! |
 |
 |
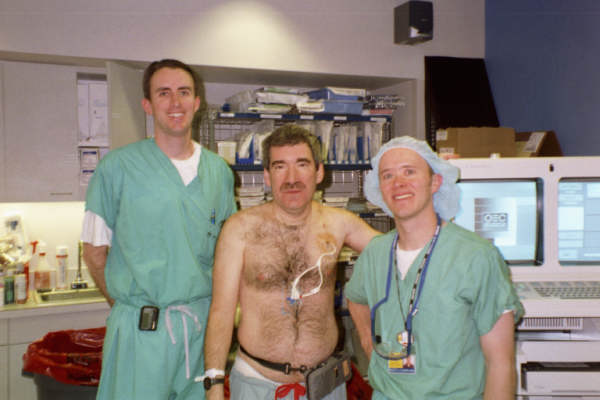
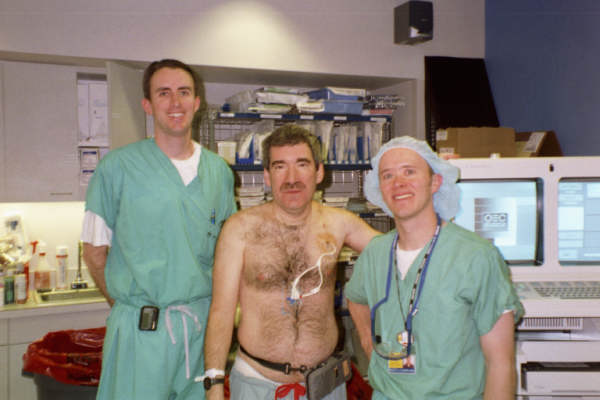
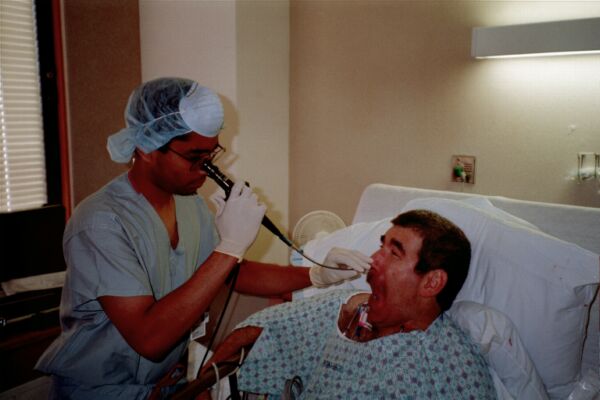
05/31/01: The AM of surgery. I am very scared. It is almost difficult to
believe that, in a few hours, I will be taken apart, have a part of me
removed, then reassembled! |
 |
 |
For me, the over-all surgical experience was hell. I remember waking up,
in the ICU, intubated. "Cough", they said. I tried, then realized there
was no way I really could, since my airway was held open. I was miserable.
|
 |
 |
The days that followed seem like a blur. Thanks to "patient administered
anesthesia", I was actually in little pain, but I was MISERABLE. I had
so many tubes in me, some of which I didn't even realize were there until
days afterwards, when I casually touched parts of my body and expected skin.
They walked me around the hospital "pods" and encouraged me to sit up as
often as I could. I was MISERABLE.
The key word here is "miserable". |

|
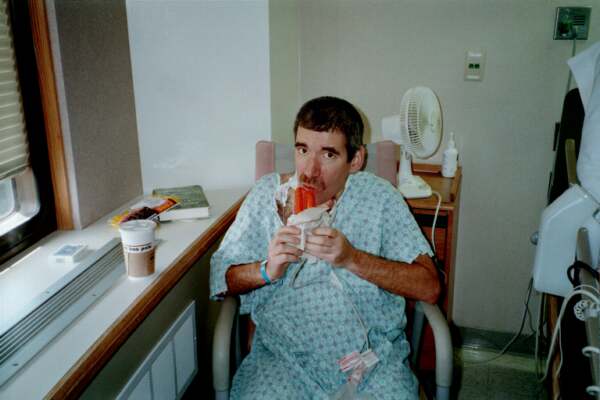 |
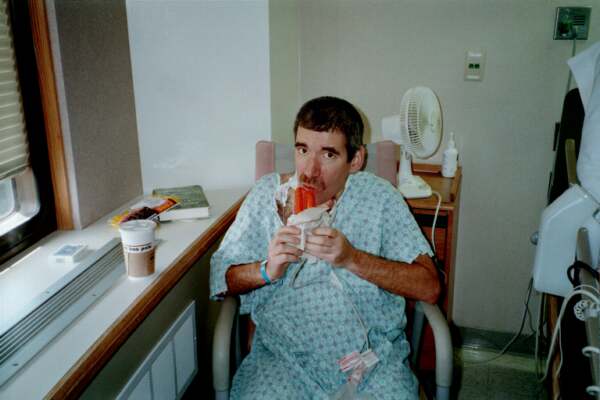
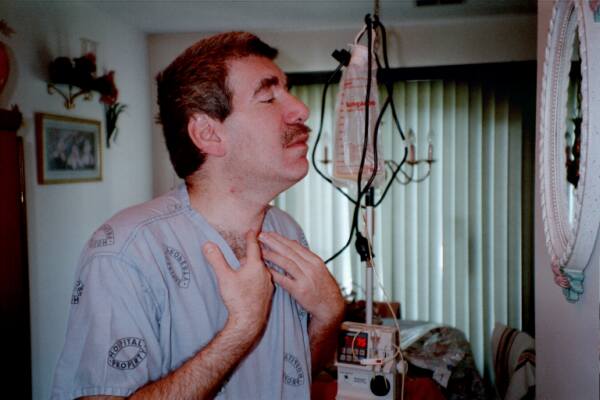
As I continued to recover, it became obvious my voice was poor, like that
of a high-pitched cartoon character. Exam showed paralysis of the left
vocal cord, which happens in about 20% of these surgeries. Everyone tells
me they ALL "get better", but it may be a YEAR or so before my voice returns
to normal. My television hosting has to be put on hold . . . . I find it
difficult to swallow, and my appetite is ZERO. Within a few days, I am able
to swallow liquids; I never enjoyed a popsicle as much as I did then! Pureed
food -- that's another story. They can paint stripes on soy product, but it
still is terrible.
Dr. Sugarbaker seems very pleased with the surgery. His feeling is the chemo
and radiation killed the tumor beyond recognition. There were no tumor
cells found at surgery, none in any lymph nodes, and the margins were
clean. He gives me a "90% chance" of survival. Now if only I can make
it through the next few months and recover. Three weeks post-op, I am
VERY WEAK. If only I could talk, and eat, and be normal . . . |
 |
 |
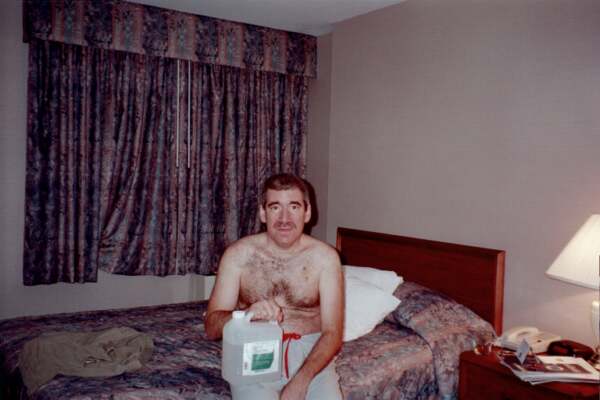
One by one, most of the tubes were disconnected. My voice was helped a bit
by an injection in the vocal cord, but was still very poor. Ten days
post-op, I was eating very tentatively and slowly, with considerable pain.
Still, it felt so good to be discharged. Like a prisoner who served his
time, they gave me the same clothes I walked in with, and told me I could
leave. The sun and fresh air never felt so good. |
 |

 |
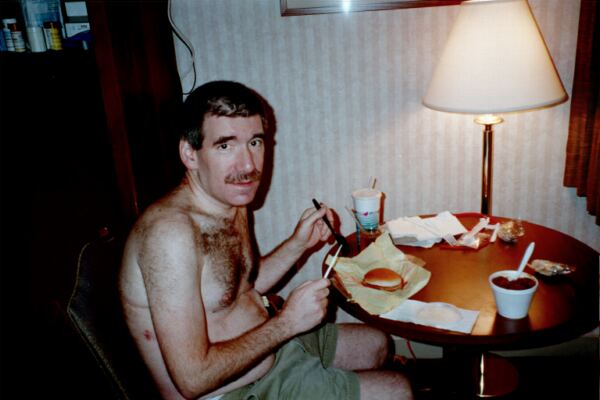
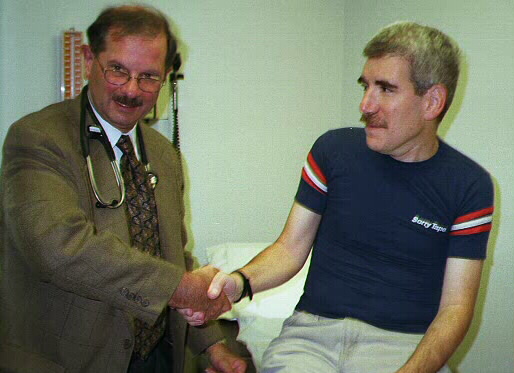
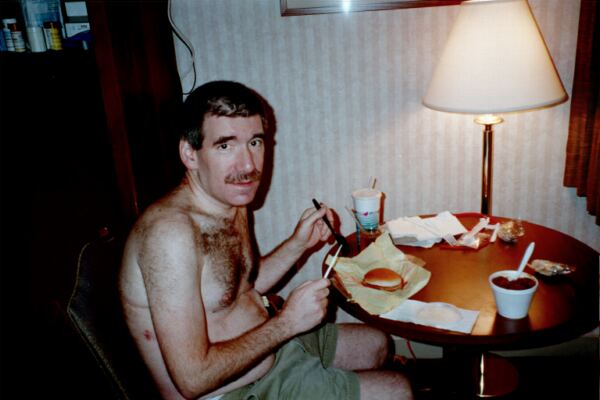
A few days later, I saw Dr. Sugarbaker in his office. His optimism ("You
beat this, doc! -- you are doing great!") is difficult for me to believe
emotionally, since I feel so weak and -- what's the word? -- miserable, but
intellectually, I am thankful things might be going well.
I felt too weak to travel home, so I stayed in Boston a few extra days.
Eating is a chore. I use a knife and fork to slowly disassemble and eat
a cheeseburger. |
 |
| RECOVERING AT HOME |

 |
Coming home was good, although the unpleasant illness followed me like a
bad penny. At times, the pain, both from the thorocotomy and from the
esophagectomy, is excruciating. It is mostly "band-like" around the thorax
and neck -- I sometimes swear someone is strangling me. Pain medicine is a
must. I have to learn how to take it -- too little, and the pain subtly but
surely worsens to the point where moving and breathing are difficult. If I
take too much, my mental status becomes "dull", which I find very annoying.
The problem is the exact, optimal dose seems to vary day by day.
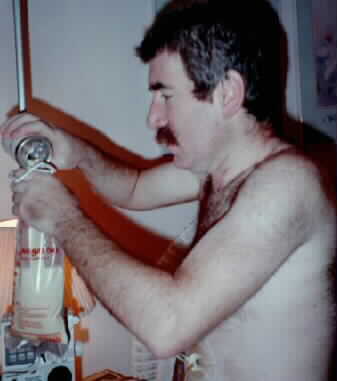
Eating is painful and I have no appetite. At night, I fill a feeding bag
with liquid that looks like pus and is described as "vanilla flavored".
The fluid is pumped in the "J tube" while I sleep, and gives me an extra
900 calories/day. (They snuck the J-tube in me during surgery!) I hate
the J tube, and the care it needs, and hope we can
remove it, thus having me "tube free", in a few weeks. |
 |
About seven weeks post-op, there are times when the pain may be a little
less. My voice might be improving. I have a persistent cough that
produces clear, thick, sputum, that everyone assures me is "normal" and
will go away ("You're doing great, kid!"). The post-op weeks have not been
without their trials. Shortly after I got home, the neck wound began to
leak fluids I had taken by mouth. Systemic antibiotics and five days of
"nothing by mouth" allowed the wound to heal.
I developed a temperature of 101 for a day or so, and had a chest X ray to
be sure I had not developed an aspiration pneumonia. Fortunately, the lungs
were clear, and the fever disappeared as mysteriously as it had developed.
The J-tube became clogged. Fortunately, this happened on a week day, and it
was easy for me to visit the gastro-enterologist, who took a pipe-cleaner
like object, and snaked the clog out! Since then, I've learned about
"Viokase" -- pancreatic enzymes -- a powder that seems to help flush the
J-tube without problems. J-tube users: ask your doctor! Physicians: call
800-742-6706 for more info. |

 |

|
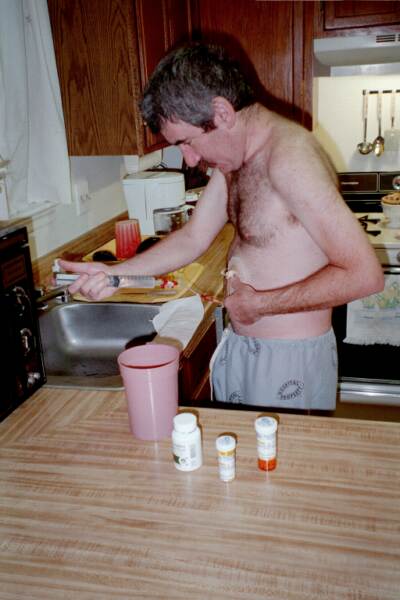
I'm now a bit over 3 months post-op, going thru the last
rounds of chemoRx. My voice has returned to probably about 95% of normal. I
have a constant foreign body sensation in my throat which makes me gag, pain when I
eat or do physicial activities (fortunately well controlled with meds), and,
while intellectually I understand the treatments are "almost over", emotionally
it is difficult to picture having my life back again!
|
|
|
By now, I had hoped the feeding tube would be out. No such luck! As long as
I'm having chemo, and have such a poor appetite, the feeling is the tube may be
providing life-saving nourishment. The deal may be worth it, but I HATE the ritual
of preparing the "food" and cleaning the tube. I'm looking for a word again . . . . yes, MISERABLE.
|
|

|
And the appetite . . . These last months of chemo are proving very difficult, if
only for the constant appetite level of -5 at best. I find even the Marinol doesn't help
the nausea as much as before. I could easily go without eating anything at all.
I sometimes remember food tasting good, but now it could be cardboard for all I
care.
|

|
|
My visits with my doctors are always encouraging. All studies so far continue to
show no signs of any cancer. Everyone couldn't be more optimistic. I can't wait to
realize the good life they all predict that someday will be mine.
|

|

|
09/18/01 was the last day of chemo. Even though I tolerated the Taxol well
in the past, it was not as easy this time! I was constantly nauseous,
and my pain tolerance seemed lower. I think after about ten
days off chemo, the "fog" is beginning to lift and I'm slowly improving, but not fast enough for me. I can't wait to get my
life back!!
For the last day, I brought cake for all the departments who were so nice to
me during the past 6 months. They were great - they all worked hard help me
make the best of a bad situation - but, hey, I hope I never have to see them again!! Its nothing personal . . .
|



|

|
October, 2001: CAT scans continue to show no metasatic disease, although
the doctors warn me not to be too happy, since problems can appear later.
As I am able to eat, I can FINALLY remove the J-tube! For essentially the
first time over 6 months, I have no tubes sticking out of me! I can take
a shower without Saran Wrap. THAT feels good!
|

|

|
I finally venture into my office. This year, Janet, my office manager, showed
the true colors I've always known she's had. She has a kind, pure soul and
demonstrates that being a good person is its own reward. Her loyalty brings
tears to my eyes. The day she came to work for me, somebody up there did me
one of the best favors of my life.
It was great to see the OR nurses, too. They still remember I like the room
cold.
As I start to see patients, I'm thankful I haven't lost my skills. My stamina
is much less than before, and I'm seeing only a few patients/week, at
most. Still, I LOVE it!!
|

|
|
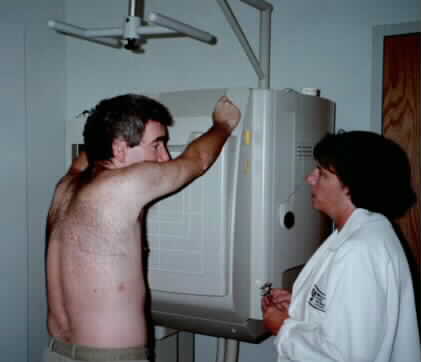
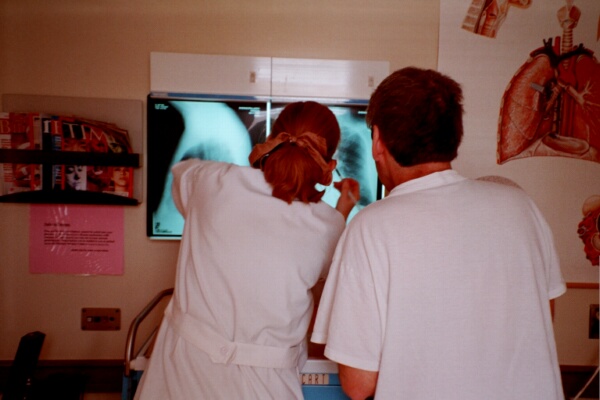
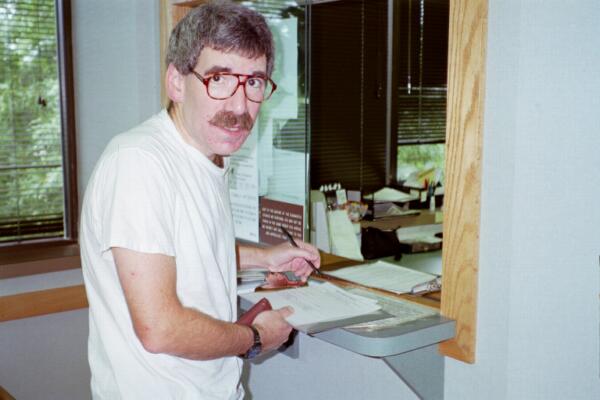
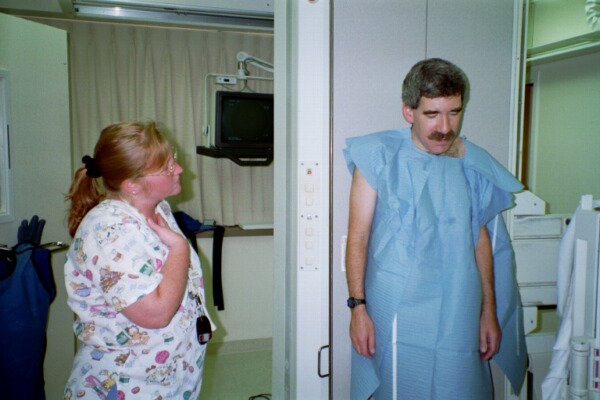
late October, 2001: About 5 months have passed since my surgery. I still require significant
medication for both post-throacotomy pain and GI discomfort whenever I eat
even small amounts. I'm impressed with how the narcotic is still able to control
the pain, though, and how well the drug does not alter my mental status.
Traveling to Boston after the September 11, 2001 attacks is somewhat more difficult,
but everyone seems happy to see me. At left, I'm registering for my usual X-ray, and,
at right, a physician in the Department of Thoracic Surgery reviews the films and
examines me. Everyone thinks I'm doing well.
note: During the past 4 - 5 months, it has
become increasingly apparent that once I left Boston, the Office of
Thoracic Surgery virtually abandoned me. "Out of sight, out of mind". To get even simple, routine forms
required weeks of phone calls, letters, and faxes. I found their "prescription
renewal line" to be inoperative, and phone calls/e-mails/faxes to staff members
were simply ignored.
What does this mean to you, as a (prospective) patient? While I was in Boston,
I think I received excellent care. Dr. Sugarbaker's enthusiam gave me hope, and
his skills (I hope!) helped save my life. But when I left, the Office
ignored me. Had I not been a physician with resources of my own, the lack of
follow-up would have been devastating. So, if you decide to use Boston, make
sure you have plans for follow-up care elsewhere.
|
|
|
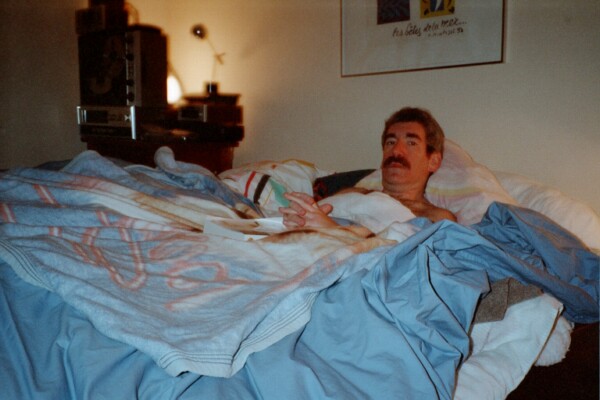
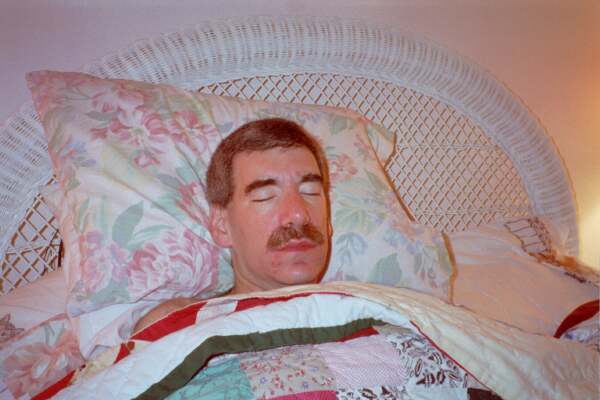
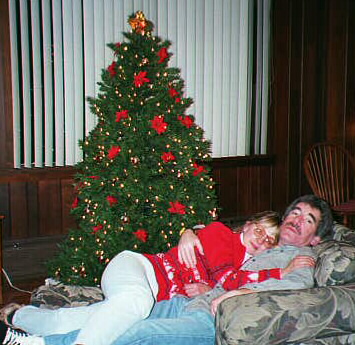
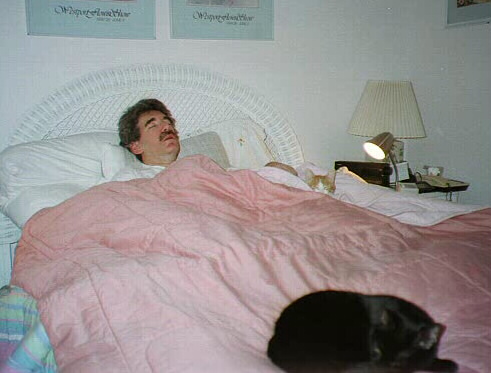
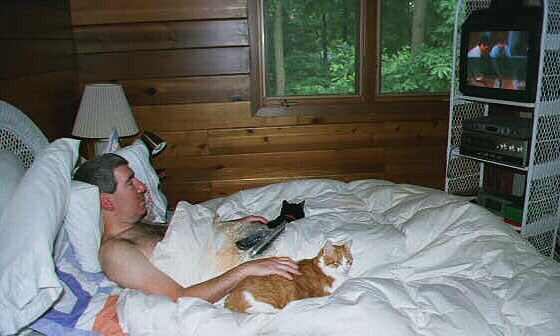
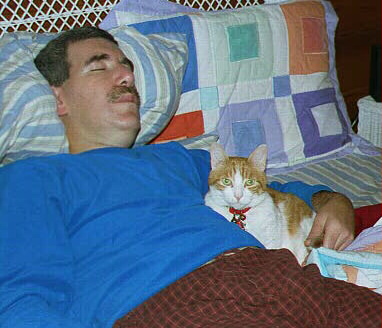
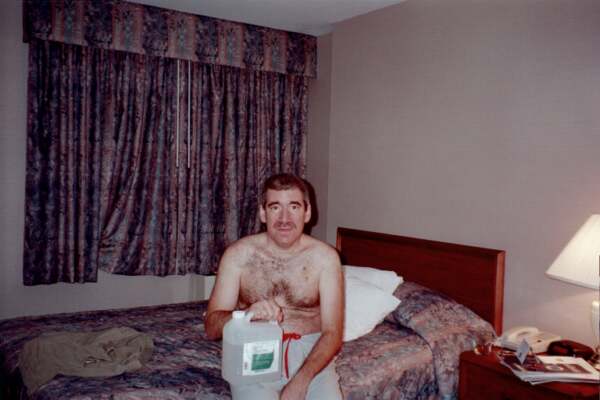
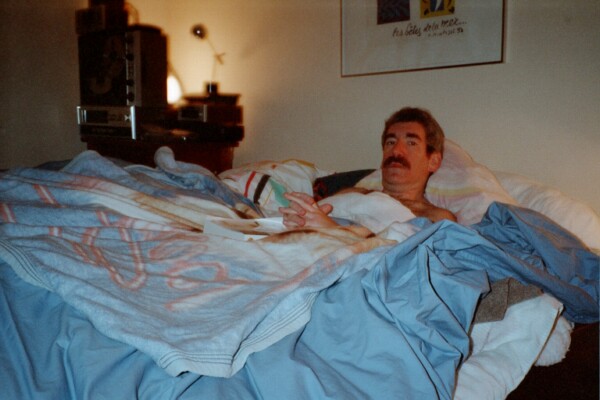
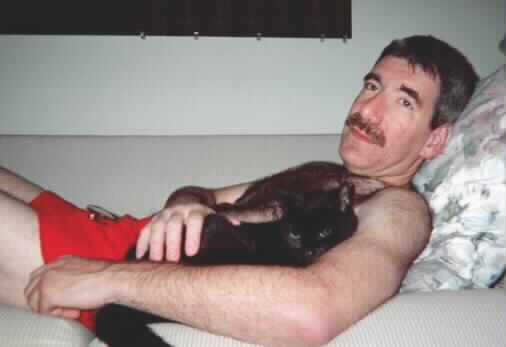
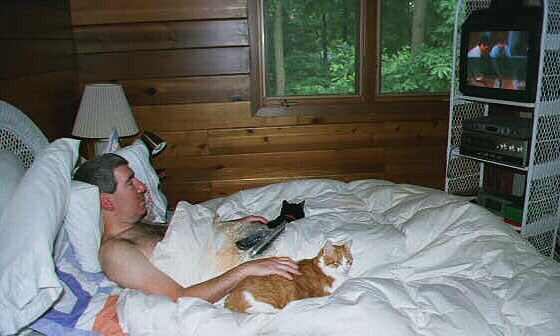
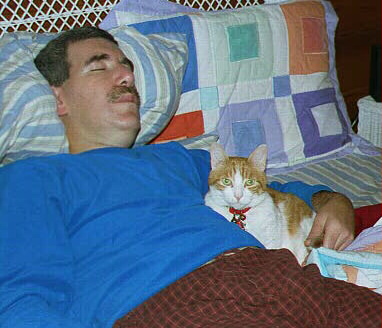
12/01: Its been over 6 months since I've been in my own waterbed. It felt
even more comfortable than I remembered it!
|

|
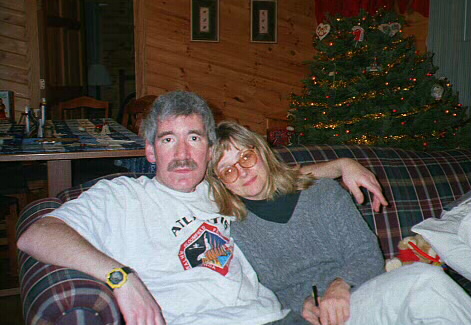
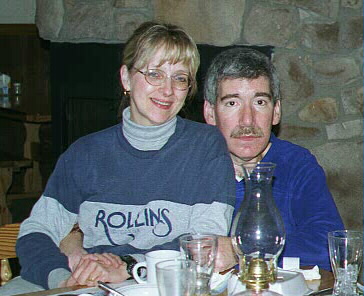
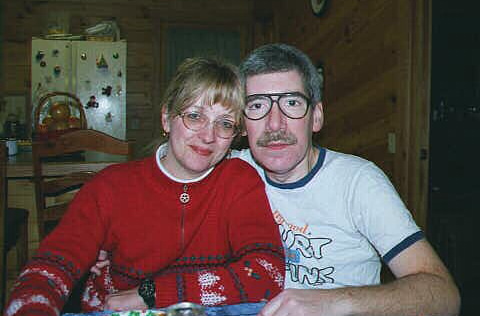
Christmas, 2001: What a year 2001 has been! Eating is still a chore, and the
pain sometimes wears thin. But I'm working on it.
They say if you make it five
years, you make it forever, so its "one down, four to go". Keep those fingers crossed!
|

|
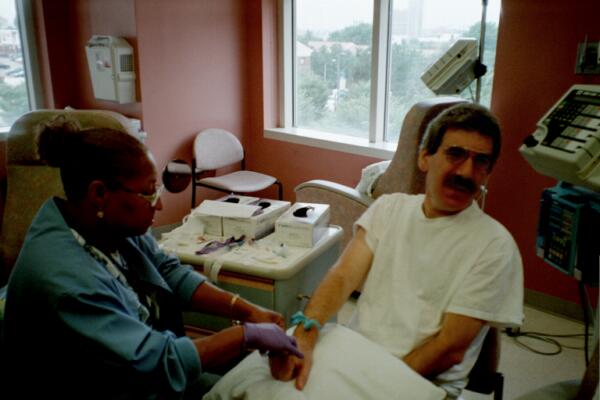
January, 2002: the first of many post-op scans, looking for metastatic disease.
These were negative, so that's good, but they tell me the positives don't
"peak" until about a year, so I'll be happier when the next ones are
negative, too!
|
|

|
|
Now, half a year post-op, my main problems are pain and stamina. They say
it takes year(s) for one's stamina to return, and the only treatment for that
is time. Pain treatment has been surprisingly difficult to obtain. Narcotics
have been the only class of agents that help me, but, for reasons I
still don't understand, they are often inadequately, improperly, prescribed.
Thinking Hopkins would be different, I requested
a "pain consulation". My request was simple: I wanted them to share their
knowledge, and provide me with the tools to help me get on with my life.
I explained that eating "small meals", "less sugar", "more sugar", or
"relaxing more" didn't help and/or were inconsistent with my lifestyle.
Can you believe it? They had the arrogance and ineptitude to come back and
suggest I repeat studies that we already knew were non-contributory, "watch
my diet", and "try and relax". You would think I was asking them to fix it
so I could drink a fifth of vodka for breakfast, when instead, all I want
is a bowl of Trix. I want to concentrate, without pain nagging me.
For all the supposed sensitivity to patients' pain this institution claims
to have (they offer patients red cards to show their physicians if they
are in pain), their consult gets an "F". (oncology: "A"; pain management: "F")
The consult was a waste of my precious, possibly limited time. What's worse,
I'm sure they think they did a good job, while the patient, me, was left alone,
to fend for himself. Other patients obviously continue to suffer needlessly.
|

|
As luck would have it, across the street from my office is a "pain management"
practice. The difference was night and day. They showed compassion and respect
for my needs and desires (it is, after all, my life), and with a
relatively slight adjustment in my narcotic regimen, there is a world of difference.
Why the "experts" at Hopkins couldn't prescribe narcotics to help me, or at least
suggest someone who could, remains a mystery. And how they could ask me to continue to fight,
if I have metastatic disease, without pain control, is beyond my comprehension.
|

|
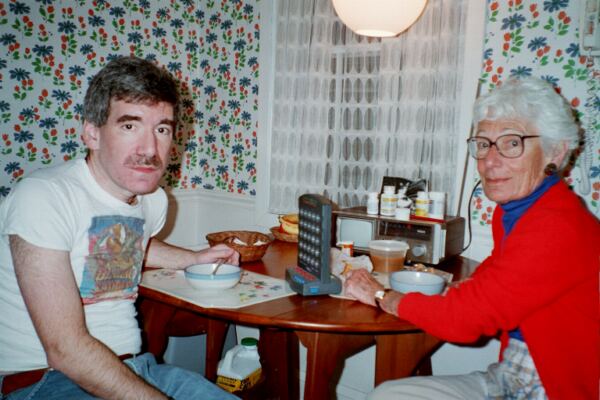
With pain control, I can share soup with my mother.
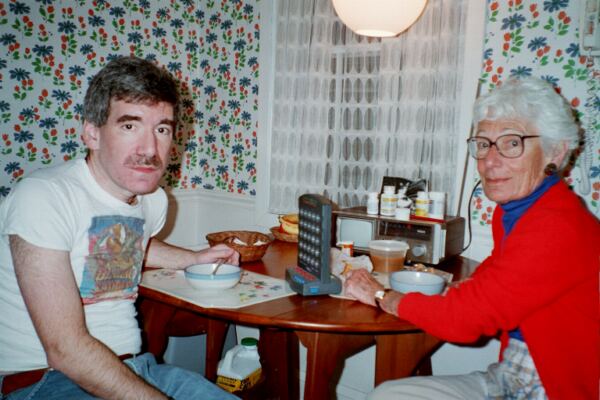
|
|
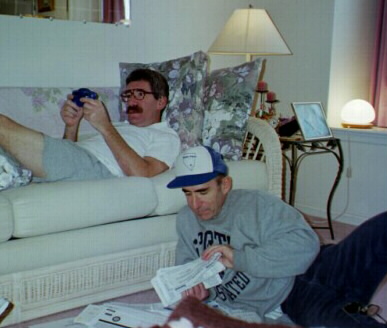
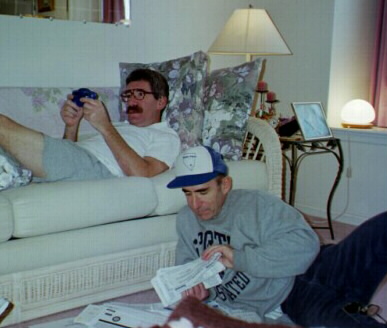
Written Memorial Day weekend, 2002, about a year after the esophagectomy:
I admit I am an impatient patient, but I have never known such profound fatigue
as I sometimes still have. I am able to perform surgery and see a few patients
(When the LASIK tech passed me my instruments, I felt like a fish back in water!)
but now I pay attention to "getting my rest". I never was a "take a nap on the couch"
kind of guy, but now, I try to do so daily. Hand-held games are very relaxing.
Eating is still a chore. Food could still be cardboard for all I care. Interesting
observations -- some foods thought of as "heavy" seem to be the best tolerated: cheesebugers,
Strombolis, etc. And, I have something I can imagine as being close to an appetite
at 2 or 3 AM!
I remain grateful for pain meds! The post-op pain remains; without pain meds, I
would suffer terribly. With them, I can function. I shudder at the thought of
patients being told their pain "should be better", and, because they can't
advocate for themselves, remain under-treated.
I continue to appreciate my family. Their unwavering support is wonderful. Remember:
You have only a finite number of "Mother's Day"s left!
|


|


|
The "year 1" CAT scan: I still can't believe a YEAR has gone by. Going back to
Baltimore is like re-visiting a bad dream. Only I'm still in the nightmare!
The people at Hopkins all remember me. I'm the "doctor who is always taking
pictures". After the usual blood sticks, IV starts, and CAT scan, I get
the news: the scan is negative. This, of course, is very good. A majority of
patients who show metastases do so by now, and the longer one goes without them,
the less likely they will show up at all.
I still struggle to "get my life back". I had hoped by now, I would be "normal",
but I'm not. My stamina is still poor, my appetite is zero, and pain with eating
and after the thorocotomy continues. I'm not a patient patient! I want my life
back, hectic schedule, long hours, poor eating, and all! I had planned to "slow down"
sometime, but not yet! My hope is my improvement will continue, just more slowly
than I expected. Sometimes I have to wonder.
|

|

|
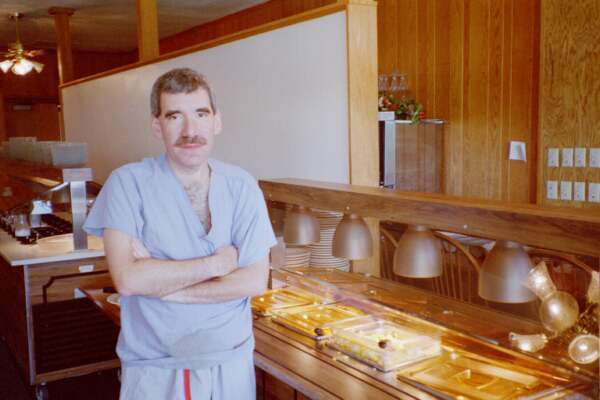
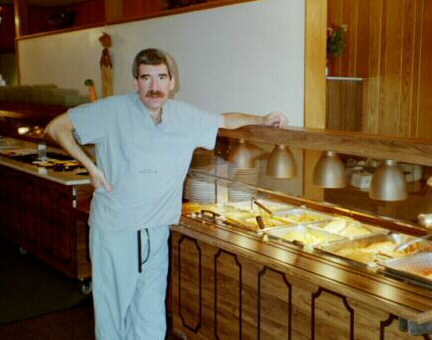
July, 2002, almost a year since the last chemo. I went on
vacation, and expected, I think, a vacation from the illness. I used to
enjoy breakfast at an "all you can eat" buffet, but this time, eating even a small
amount put me in excruciating pain. A hot dog at a picnic makes me uncomfortably full.
Its very difficult to predict just how much food I can eat, and when, but generally
extra narcotics and rest helps. I'm glad food was not a hobby, but, man, I miss the buffet!
My stamina remains poor. I want my life back, but still don't have it. I used
to be able to work 14 hour days, do work at home for a few hours, sleep for
2 - 3 hours, then look forward to repeating it the next day. While I may
have felt "tired", I never felt "sick". Now, if I try to work anywhere near my usual
hours, I become physically ill. I'm thankful that sleep and "relaxation" help.
In medical school, I never learned WHY that should be the case, and I'm very
curious.
|

|
|
I had hoped by a year post-procedure, my eating and pain would have improved.
Instead, eating can be VERY painful, and I still cough up annoying saliva.
Getting a barium swallow and associated studies should be straighforward, right?
Instead, I'm seeing the erosion of medicine. The workers in the radiology
office seemed burned out and simply didn't LISTEN. Example: I needed
more than one copy of the study, but it was obvious my repeated requests were falling
on deaf, non-caring, ears. After the study, when I asked for copies, the
only thing the radiologist could say was "Gee, I'm sorry, I didn't know you
needed them".
In any event, there was an obvious constriction
at the level of the diaphram.
|
|


|
My struggle with the medical establishment (not to mention my GI tract!)
continues. Hopkins had me drive 50 miles to Baltimore for a 7:30 AM appointment,
only to turn me away because the doctor wasn't available. Not once did
they make any effort to contact me before my trip! I thought the second appointment
would go better, but I again returned empty handed because this time, there was
no anesthesiologist. For the third time, I personally saw to it that
everything was on my chart, only to be told I had to be there 6 hours
before my procedure. Why? No one would look at my chart before my appointment,
and they couldn't care less if I spent a day, away from my life and home, in pain,
needlessly doing nothing, waiting. Sure enough, the AM of the procedure, in less
than a minute a P.A. determined my chart was in order. I could sit wherever
I wanted for 6 hours until they were ready for me!
As usual, I felt the physicians themselves were top notch. I'm embarassed to say
I don't know the name of the anesthesiologist, but I didn't feel a thing! And I
have no doubt Dr. Canto did an excellent job performing the ultrasound and biopsy.
The results of the study were good news and bad news: the good news: no
cancer. The bad news: no fixable pathology to explain the constriction and
thus the pain. I expect to be on narcotics for the foreseeable future.
I'm seeing medical administrations deteriorate before my eyes. Institutions
that purport to help patients fight cancer shouldn't make the patients fight
THEM, too! Self advocacy is very tiring . . .
|





|
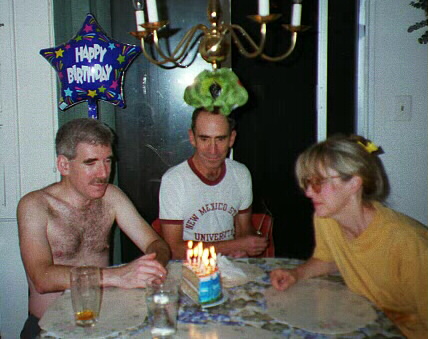
|
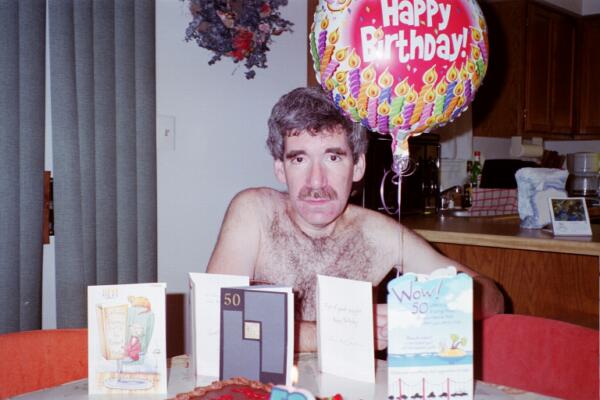
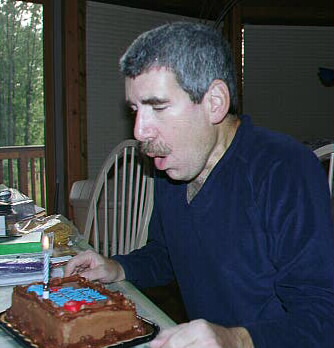
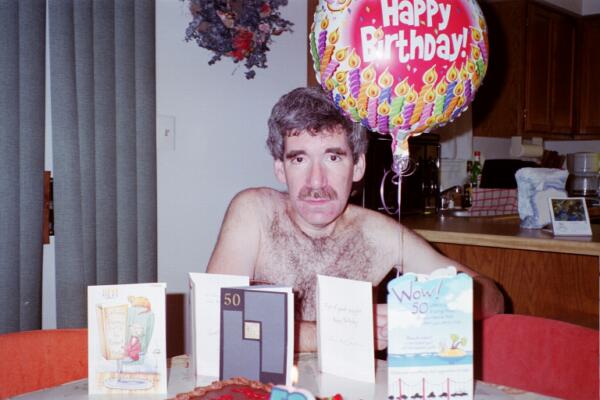
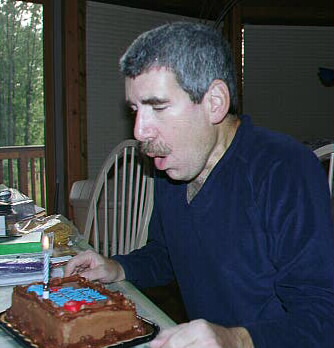
When I was a kid, I thought 50 was old. I don't feel like an old person.
And yet I almost didn't make it! Happy Birthday to me! Don't worry -- I plan to
make 51!
|
|

|
Fall moves into Winter -- its now almost 2 years since this
ordeal began. My life is still far from normal. Eating remains a painful,
unpleasant chore. I know I have to eat, but, intuitively, it feels like eating
is bad for me. Go figure. My interests are starting to come back --
I'm starting to design projects in my mind, but I don't have the stamina to
execute most of them. I can easily sleep 12+ hours (and, when I do, I
sometimes feel better), but then the day is gone. I am easily exhausted.
And, oh, how I miss the "all you can eat" breakfast bar. Heck, I miss the
anything you can eat bar!
|
|
|
I have CAT scans every 6 months at Hopkins. Its difficult for
me to imagine how a human being can live and have so much difficulty with a
basic life necessity such as eating, yet for some reason I'm fairly confident
that the CAT scans won't show recurrence/metastatic disease. Thankfully, the
studies remain negative.
|
|
|
Christmas, 2002! There were those who said I wouldn't be here,
but I made it. Its a tough road. For Beverly, I'm sure, as well as me. I'm
fully aware that most people with this diagnosis would be dead by now, but
last year, at this time, I had hoped I would be more "back to normal" --
that somehow, I would look back at all this, and say, "man, that was terrible!".
But now sometimes I fear that my life will never be what I once so much enjoyed.
Thanks in large part to the encouragement of my family, friends, and, yes,
sometimes my patients, I go on. And, yes, there are times when I feel O.K.!
|


|
| Time flies. Its over 2 years since this whole mess began. If
my improvement continues, its too slow for me to notice. I feel like I'm reaching
my "steady state", and appreciate humans were born with stomachs for a reason!
Yes, I can see a patient, but if I see several patients,
I become so fatigued I feel like I'm fighting death. I have never known such fatigue.
If I rest, sometimes I feel O.K. Hmm . . . if I could get a job as a mattress
tester . . . . .
|
|

|
They say one of the most stressful things you do in life is buy
a house. I agree. But my fiancee has wanted a house for both of us to comfortably
live in, for years, and she found one that she likes. It kind of looks like
a cabin in the woods, but I'm assured I can have cable and a TVRO dish. But I
hate dealing with the real estate people. At least my doctors acted in
what they thought was my best interest. The real estate people on the other hand
say and do anything to get money, and not being able to trust them drives me
crazy. Its almost difficult to believe. Look at the bespectacled meanie on the right side of
the lower photo in the right column. Example: Day 1 - I observe soot in the
water and complain. Day 2 - the dishonest sourpuss tells me "the water is now running
clear". Day 3 - at my insistance, against the dowdy frump's will, I have a
plumber examin the house. Soot still in water, always was, still is. Somebody's
lying. Believe me, I would walk away from these creeps, except that I view
the house as an investment in the happiness of someone who has proven herself
by sticking with me during these hard years.
Dealing with the real estate people has taken a lot out of me, and has been hard
on our relationship. I still worry, hopefully needlessly, that I don't
have the stamina to operate a new house, espeically one that needs this much
work. Time will tell.
|

|
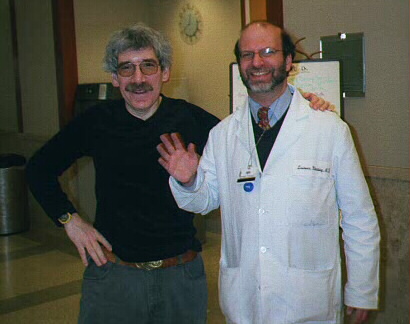
| It is now about 2 years since the radical esophagectomy, and I
still have little energy. I require pain medication to eat and function. At
left, I tell this to my oncologist. Her reply: "You are a [drug]
addict, and should be in a rehab program". How cruel! I couldn't make something
like that up if I tried. Another example of a physician who is presumably excellent
in a subspecialty area, arrogantly, erronously, thinking she knows it all.
Patients needlessly suffer.
At right, I have the 2 year CAT scan.
|

|
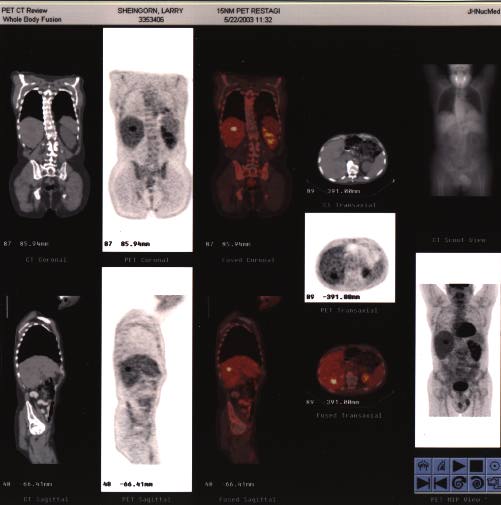



|
My worst fears are confirmed. The halls and exam rooms that once
gave me hope now seem more cold and sterile than ever. Various scans show spots
on my liver. I feel better, in a way, knowing that the suffering I'm going through is,
in fact, NOT normal. But the thought of leaving loved ones behind, with so much
to do, so much to learn, so much left UNdone breaks my heart. At this point, I
have between 6 - 24 months to live. Death from this disease is certain.
Hopefully, my doctors will work to keep me comfortable, and make my life as good
as possible, but the fact of the matter is I feel like I have to take care of
even that myself.
The hell begins again. The countless forms, the repeat scans, and this time,
a liver biopsy and ultrasound. This go around, I've decided the tests will be fewer;
I will not spend my last months under the care of people who have so little
empathy that they dismiss me as a "junkie". I'm at a loss for words (not to worry,
I'll think of something!), but, as I say, there is a sense of relief.
I just can't picture my family, my cats, my friends, my house, Christmas vacations,
Twilight Zone re-runs, train rides to work, the world, without me, but, of course,
they all will go on.
|




|

|
The trip to doctors begins. It took about 45 minutes to get the name, address
and zip code on my registration form correct ("Its not my fault, someone
else entered this data wrong", etc.). Dr. Steves at the Washington
Hospital Center was very nice and seemed knowlegeable. So far, the plan seems
to be "radiofrequency ablation" of the liver tumors, followed by more chemotherapy;
I can always stop the chemo if it makes me sick and/or it does no good. The
chances for chemo helping are about 30% or so.
I continue to be comforted by the "pain management" people, who promise me
they'll see to it I get "whatever I want". As expected, I seem to be building
tolerance to the pain medication, and their words reassure me I won't suffer
needlessly.
And, of course, my family. My friends and loved ones seem even more important
to me now than ever before, and I'm blessed to have them. I hope I somehow live
on in their memories, and maybe even in the relationships my life might have
created between them.
|


|
|
I'm trying to simplify things a bit. I've got a good oncologist who is closer
to my home, and I reveiwed the "bad news" scans with him. He agrees that radio-
frequency liver ablation is a reasonable option, keeping in mind the quality
of life vs. longevity issues. I decide to go ahead with this procedure, then,
in mid-July, see the local oncologist again, who, working with Hopkins, will
decide if chemo is reasonable soon, or if we should wait until new metastatic
lesions make themselves known.
As painfull as it is, I have to plan for the possibility of me being sick after
the liver procedure, and from the chemo. While I may continue producing
television programs, because of my uncertain future, I can't commit myself for
future shows. During the past few months, my friends at the TV station did much of
my work, and I can't continue to impose on them. I cried, on air, when I said "goodbye"
to the viewers of one of my TV shows, The Doctor's In, and "got my affairs in
order" at the lawyer's office.
|

|

|
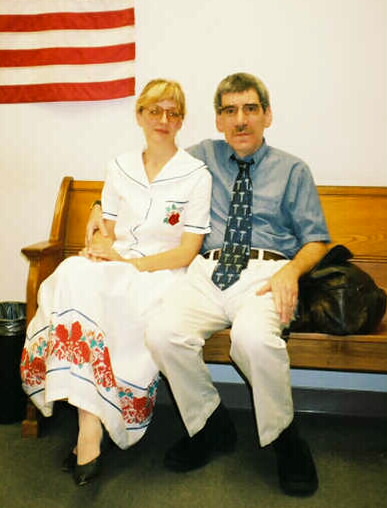
It was obviously time for me, at long last, to marry the woman whose
loyalty is unquestioned. She is my best friend, and only wants me
to get better. I owe her my life. Our wedding date: June 23, 2003. We
drove to the courthouse and signed the papers.
|


|

|
It was then onto the radiofreqeuncy liver ablation. Even though I tried every
way I could think of to be sure the doctors knew I needed large amounts of
narcotics to control my pain, it didn't work! I was in more pain after the
liver ablation than even after the radical esophagectomy. My liver was so
tender I could hardly breathe! It took about 36 hours to have the "pain service"
do the obvious and increase the dose of the narcotics -- I felt better in
about 30 minutes!
|


|
|
And now the next thing: should I take more chemo? There are different opinions.
Some feel that, since I have no detectable cancer, why not leave me
alone until new lesions make themselves known? In a way, this appeals to me,
since, as I slowly recover from the liver manipulations, I feel pretty good!
On the other hand, it makes theoretical sense to try and kill whatever tumer
cells may be around while they are low in numbers. No one is promising me
a cure -- no one really knows, I don't think, the effect these medications might
have. On the one hand, I want a good quality of life; on the other, I want a life,
period! So, with much ambivalence, I decide to try at least a few rounds of
taxotere and CPT11. Stay tuned . . .
|

|
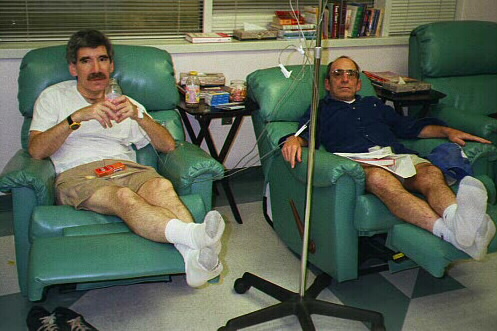
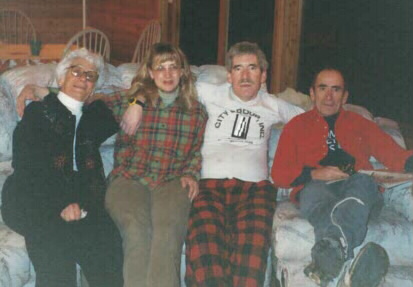
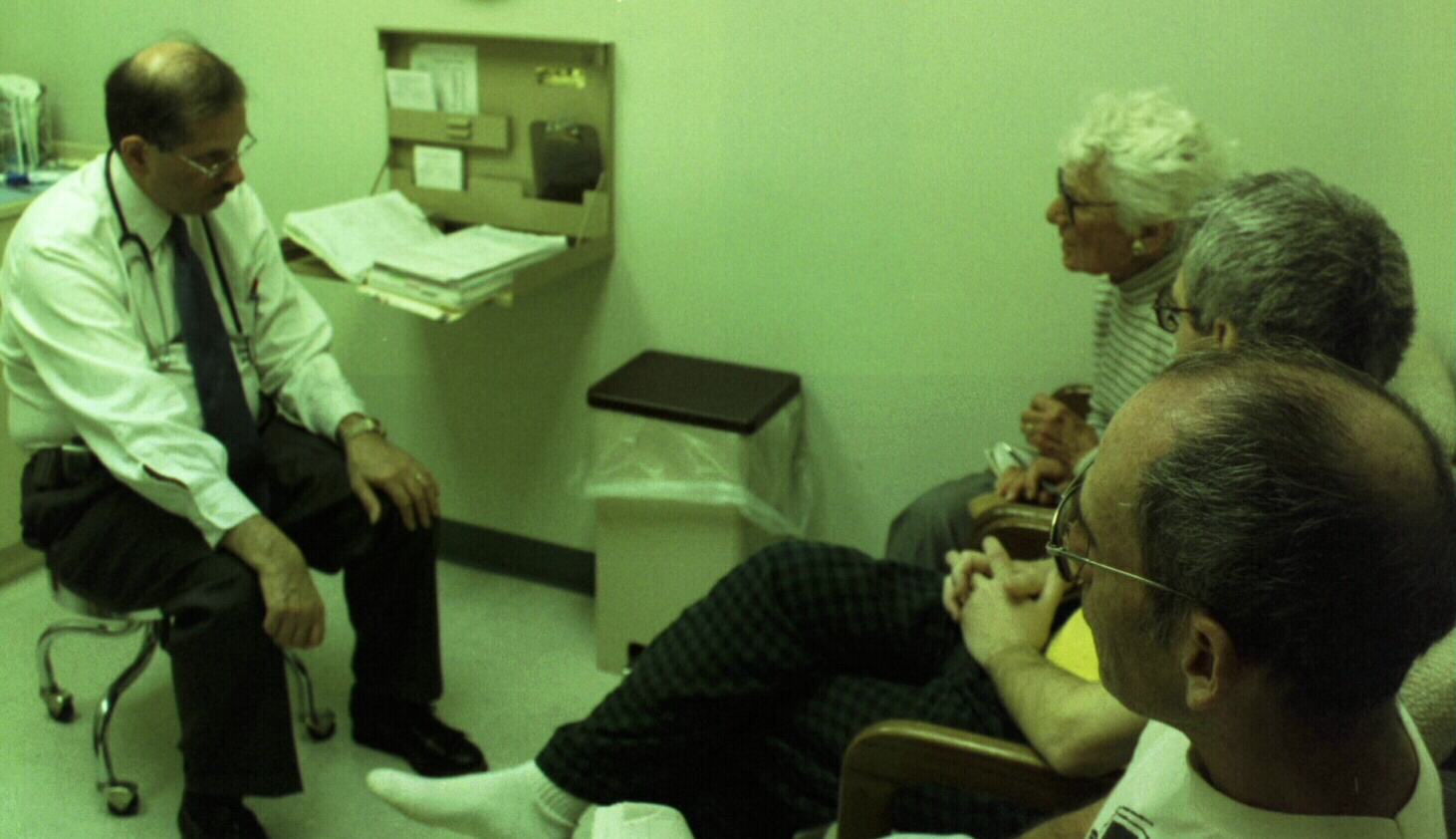
My local oncologist is proving to be patient, compassionate, and, I think, skillful.
He spends hours with me and my family. I am glad to be able to have more of my
care closer to home, but the situation is not good. It "would be
a miracle" if I was alive in 4 years. The doctors honestly feel a few rounds of
chemoRx might help me live longer, and, might keep me alive long enough to
take advantage of possibly as-yet-undiscovered treatments for this cancer.
I can't explain it, but it is so comforting to have my family with
me during this ordeal, even though all they can do is sit next to me and talk.
|
|

|
These rounds of taxotere and CPT11 are more difficult for me than I remember past
chemoRx's being. I thought I would be able to work during most of the treatments,
but I am just too weak. For a while, my hair "came out in clumps" (see photo of
bath drain, at left), but this stopped before all my hair was gone. There are
some days during the chemo treatment that I am so weak I can barely get out of
bed. I feel like I am dying, and, if life were like this, I would not want to
live. The oncologist assures me, though, that everything I'm feeling is expected,
and will improve once the chemo is done.
I've made the very difficult decision to sell my practice. Ophthalmology has given
me everything I've ever wanted, and more. I have had the privilege of using my
technical skills to improve peoples' quality of life, and have been able to make
a living at it, too! Words can not express my gratitude to my patients for their
trust. I have been blessed. But even if I do recover from the effects of the
current chemo, the cancer is expected to return within a few years, and I will
probably be back at square one. Life without the responsibilities of my practice
will be easier to manage. The decision brings tears to my eyes, but seems the
only rational course of action.
|

|


|
The past three months have been some of the most difficult times of my life.
This last round of chemo was the hardest. Even though intellectually I knew I
was supposed to feel tired a few days after each treatment, emotionally,
I couldn't "remember" that I would feel better soon. Some days I was so weak
I could hardly dial the phone (that is Moe in the picture). My wife kept a "log" of how I felt
each day. The oncologist, and his staff, were all wonderful -- they encouraged
me to keep going, and continued to point out that I have a "slow growing" tumor.
I might live a "long time", they say, but when I ask them "how long is long?",
they have to admit its only a few years. At the end of the chemo, I couldn't
help but remember that I've been here before, thinking I would never be back.
This time, if the tumor recurs soon, I will probably do nothing. This last treatment
cost me three months of my possibly very short life.
I have cried many times, when I think about leaving my patients and my practice.
If there was ever a doctor who worked harder for his patients, who sweated
the details, and who cared about them more than I, I haven't met him. But
leaving my practice is the only sensible course. I am too weak, even now that
the chemo is done, to do the practice justice. I sat on the deck of my new house (nope!
haven't moved in yet!) and gave the matter much thought, listening to the same radio
that played during gross anatomy dissections in med. school, the same radio that opened
my father's office, just as it opened mine, too. I will miss my patients, and my staff, more
than they will ever know. But its time for me to step down. I leave my practice
thinking it was a job well done. I have been blessed.
I am grateful to my wonderful family. We were always very close, and I don't
think I would be able to get through all this without them. They sat with me
while I was so weak I could only complain and fall asleep, and they were still
here when I awoke. We took walks, we had soup, and we talked.
|

|

|
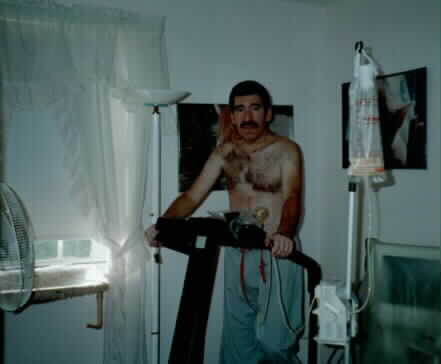
My wife prayed for a negative scan after this latest bout of liver surgery, and
chemo, and, as expected, it was normal. The reality continues to set-in.
I know I am dying. I can't explain premonitions I have. I feel unmistakably
"not myself". I am weak, yet, objectively, I tolerate the treadmill and working
on my house. I expect my stamina to slowly improve, until the cancer appears
again, but am sad for the parts of my old life that I'll never have again.
We signed papers officially transferring my practice to Tony Roberts, M. D., as of
January 01, 2004. I'm sure he is sick of me telling him how lucky he is, but
he knows I feel lucky to have him, too! My patients will be in good hands,
and that is a huge emotional relief.
|

|


|
For the past 20+ years, the end of the year has been a time for me to close my
office for 2 - 3 weeks, look back on the year's work, appreciate what the year
has given me and allowed me to do, and prepare for the next. The 2003 holidays
are different. I had to hold back the tears as I saw what I knew was my last
patient, and, even though I am glad Dr. Roberts will inherit my practice, I am
very sad to say goodbye.
As of early January, 2004, we are just moving into the new house. We had Thanksgiving
dinner there, and, finally, I see the house taking shape. Things are still too
busy -- closing my practice is very taxing. When I'm done, I
plan to spend more time with my family and friends. They are very important to
me, and stand by me, even though my career has prevented me from giving
them the time they deserve.
|

|
|
I look at the Christmas photos from 2003 and see myself, now obviously middle aged,
with gray hair. The years have taken their toll. I've said this before: I just
can't picture these activities going on without me, but they will, and I will
be only a memory.
|


|


|
In a way, time flies. It is already near the end of the first quarter of 2004;
doctors told me I would be dead by now. We still continue to move in, and set
up the new house -- doing so is a lot of work. Every few weeks I find another
"secret" that needs repair, and I'm glad I'm somewhat handy so I
can at least understand what the problems are! Its obvious that I will enjoy the
house once we get things set up. The view from the balcony is sometimes like
a picture post card. Now, there is a (temporary) lull in things that need to be
done. I never was a morning person, but I note I feel "sick to my stomach" when
first wake up. I often sleep 'till noon, and find the narcotic very much helps the
AM discomfort.
It is very strange sleeping late every day. All my life, I got up early, and
was part of the hustle and bustle of working life. Now, I see people at work
and wonder how I ever did it! And, sometimes I feel like a man without a home.
My workbench and tools are still at my old house, waiting for the new addition
to be completed here. Yet many of my things are here, at the new house.
The only one who feels completely at home, I think, is my cat, who has a small
house in the living room. As far as he is concerned, he's home.
|

|

|
This quarter's scan continues to be "negative", showing only the expected
resolving liver lesions after the ablation. I hate going to Hopkins for those
scans. People are officially polite, but its obvious many of them are "burned
out", through no fault of their own, and the human contact that drew me to
medicine in the first place, is gone. And I can't find a single physician who
has seen someone like me not die from this disease. So, when I have these scans,
it is like "waiting for the other shoe to drop". My experience with chemo/radiation
and other treatments has been so difficult that, if the lesions return, I
honestly don't know if I would ask for treatment.
Perhaps an
exception to the doom and gloom atmosphere is the radiologist who participated
in my care. Similar to my oncologist, he reminded me that my cancer is very slow
growing, and similar GI cancers HAVE, in fact, been cured, so anything is
possible. Still, I wish I could bet on it!
|
|


|
A month or so ago, I noticed a gradual swelling in my scrotum, which became
increasinly painful. Thankfully, it was a benign process, unrelated to the
esophageal cancer, which was repaired as a "day surgery" procedure.
Even so, I HATE being a patient. I HATE the "goodbye" as they take me into
surgery. This time, I felt very sad during the post-op days. Maybe the surgery
reminded me of what I might experience when/if the tumor comes back. And, I suspect I irrationally thought the
acute surgical repair would somehow improve the esophageal cancer pain, which,
of course, it did not. Then, there ARE reasons why it is rational to be sad,
I suppose. When I talk to my old staff, visit my old office, and even go to
doctors' offices as a patient, I miss being on the inside. Parts of my life
will never be the same. Am I "depressed"? I don't think so. I sleep well, and
can concentrate, but, so far, I haven't started major projects like I usually
do. On the other hand, I think I will very much enjoy having my workbench when
the new addition is complete, and plan to shoot television shows in about 3 - 4
months. Even so, one of the nurses (right) suggested I try Zoloft, which I started last week.
It takes a month or so to see any effect, so, I'll keep you posted.
My brother takes "road trips" for days to a few weeks, and I'll probably go
with him during the next few weeks. I can't emphasize how much my family helps
me through these times; I couldn't do it without them.
|


|
My first year of retirement started out with me working on the new house. This
keeps me very busy. I wonder how I ever worked as hard as I did, while doing all
of my other activities, too! I do not think I am clinically "depressed". The anti-
depressant made me feel much worse; when I stopped it, a cloud was lifted from
my brain. I am concerned, though, that I still have nowhere near the stamina I
once did, and have various aches and pains that were not present when this whole mess
began. I can't do things, not because I am "depressed", but because I'm too weak,
too naucious, or in too much discomfort. The doctors view me as a miracle -- the
fact that I'm alive makes them say I'm "doing great". But "doing great" for me
means a normal life with a normal life expectancy, and I'm afraid I have neither.
Heck, I can't even eat without narcotics!
When I was working, I was too busy to see my friends. Now, I continue to travel
with my brother, and invite friends to the house on Saturday nights. My wife's
parents visit here, too, and I enjoy spending time with them. I'm aware that they
will probably be with my wife, for a while anyway, when I am gone.
Supposedly, the addition to the house will be finished by the end of August, 2004.
(I'll believe it when I see it!). The new house will be a paradise -- I
will be able to work on my electronics and computers, have a post-production facility 3 minutes
from where I sleep, and learn more about cars and wood-working tools.
Another scan will probably be scheduled for June, 2004. Stay tuned, with
your fingers crossed! When/if it turns positive, I honestly don't know what I
will do.
|

|


|
As Summer of 2004 starts, I'm still working on the new house. I'm often able
to be here while various trades work on the new addition. Thank God for
that! I'm able to have them do things just as I want them. At last! A house
with wires where I need them. I can't wait to have my workbench near.
Think of it! I'll be able
to do my electronics, study computers, edit video, and do many other things,
all in electronic comfort. The house will be very cool, and I hope it will be a good reminder
of me when I'm gone. Maybe carving my name in the garage floor cement will
give me immortality.
I enjoy sleeping late, but in many ways, retirement is very difficult for me.
The practice I built with my own two hands is still running; when I visit,
I sometimes cry. I often feel worthless. I'm
no longer a mover and a shaker; instead, I'm a guy with time on his hands.
My friends are wonderful -- they remind me of my accomplishments. I suppose
they are right, but emotionally, I can't shake it. On the other hand, over
the past few decades, medicine has deteriorated into a cold, uninviting
environment, where doctors are often angry and burned-out (sadly, justifiably
so). The profession I once loved so much has, indeed, changed, and, as
malpractice rates continue to soar, I realize
in some ways, I'm glad to be out of it.
Everyone tells me I look great, but I am often in pain, even with the meds, and
don't have the energy I loved a few years ago. I absolutely hate going
for scans and seeing doctors. After the last scan, I got the phone call:
there were several areas of "possible" abnormalities. My oncologist
says "don't worry". We'll repeat the scans in 3 months. I can only hope the
areas of concern don't represent significant pathology.
|

|


|
How's this for something completely unexpected? One day I came back to the house,
and my wife says: "look under the couch". I was tired, but I figure "OK".
I see two eyes attached to a cat, and think its one of ours. She
says "look again". Sure enough, they belong to a new cat she had
just bought! I still can't figure out exactly why she did it, but she has a knack
for finding good cats, and this one proves to be no exception. Within a few
days, the name comes to me: BOX. (Should we spell it "BOXX")?
|
|
|
During the mid-Summer of 2004, I find I don't feel so good. I have
increasing abdominal pain, and think it might represent pooror pain control from
decreasing narcotic effectiveness. I'm almost certain I'm not more "depressed"
-- I found the Zoloft actually adversely effected my mental status, and
long ago discontinued its use. During my planned visit to the oncologist, he
tells me to repeat the scan. He tells me its
very likely that at least one of the areas of "possible" concern
represents tumor spread, and my pain might be secondary to that. If so, we would
switch from seeking an unlikely "cure" to palliative treatment. OUCH!
I plan to go to Hopkins again for another scan, and will return in a few weeks
with the results. I keep my fingers crossed, but a good result seems unlikely.
|

|
Yet another trip to Johns Hopkins to repeat the scan. Much to my dismay, I found
many of the staff to be quite callous. They wouldn't let my wife accompany
me as she had done every time up to now, and wouldn't even take my picture
(of ME alone!), claiming "confidentiality" issues! Utter inexcusable nonsense.
As I've said so many times over the past decades, what they should have done
would have cost 15 - 30 seconds, at most. I'm afraid they may be
"burned out", as so many medical people (understandably!) are, but Hopkins'
arrogance is mixed in, too. After they were done, one of them disingenuously smiled, and
said "have a nice day". I replied "go to Hell". A good choice of words.
Hopkins helped me, but they don't realize they, like all of us, have a lot to learn.
I'm thankfull for their research, but unless I really need them again, I'm
spending my time and money elsewhere. I said "Goodbye" to Hopkins.
|

|
|
My oncologist reviewed the scans with me a week later. Not good. There is spread
of the tumor in the mesentery, and at least one of the liver lesions has returned.
My not feeling well this Summer was probably because of the liver involvement;
and a cure is now virtually impossible. Paliative treatment is now all they have
to offer.
I HATE being stuck for blood, and I HATE the effects of chemo. Even with all the
drugs, chemo still nauseates me. It makes me tired, and unable to think.
I'm not the kind of person that can vegetate -- if I'm not learning
or earning, I feel worthless. I've vowed not to prolong my
life with a poor quality of life. Maybe I'm being a coward when I trust the
oncologist, but he says doing nothing would be foolish. After the first round
of chemo, my liver enzymes improved -- the chemo is probably causing the cancer to
regress. With some ambivalence, I agree to more rounds of chemo. I'll go into
2005 feeling terrible for about 3 - 4 weeks,then feeling OK for about a week, then
repeating the cycle. I plan my life around packing 3 - 4 weeks of activities
into the week that I feel OK, between cycles.
Hopefully, when the smoke
clears, I'll have months of enjoyable living without the cancer being manifest.
|
|
|
Can you believe it! I made it to another birthday! 52 years old. I've worked
so hard, and have so much I want to learn and do. I'm just not ready to leave
earth yet. I'm hoping I'll see 53! Maybe in about a year . . . .
|
|
At the close of 2004, I began to notice very subtle, but I think definite, increasing
right upper quadrant abdomnimal pain, not strictly related to eating, and an over-all
generalized weakness. How do I know this? My wife told me, months ago, a switch on her car
is broken, and I haven't fixed it yet! The most recent scans were somewhat equivocal, but
MAY have shown some tumor enlargement in the liver. It is a very "slow growing"
tumor, with only minimal elevation in liver enzymes. But the associated systemic
symptoms are very disturbing.
|
|
|
This year's Christmas was very strange. Family squabbles seemed especially
selfish, obnoxious, and trivial. How can anyone get upset at such trivial
problems? Life is over before you know it. Don't they get it?
As infighting
broke out, I felt very alone. It brings tears to my eyes when I think of my wife,
perhaps as soon as next year, coming to this event without me.
Will I be able to watch over her after I'm gone? I will miss her so much!!
|

|

|
I don't want to leave the earth! Not now. I've worked so hard to get where I am,
and want to enjoy my knowledge, my wife, my interests, and my life. But I can't
see things getting better. If the pain continues to worsen, and I continue to
weaken, I see no other ending. It breaks my heart to think that my cat, Box, will
get old, and die, without me. YIKES!!!
|

|
When I don't take chemo, my liver enzymes slowly get worse, consistent with
slow growth of the metastatic lesions that will soon kill me. My oncologist
spends as much time as I ask with me and my family, but really, what can he say?
What can anyone say? We are closer to the end of the line as far as conventional
treatments go. Currently, I'm on a chemical that has a 20% chance of reducing
the tumor. I've taken it once, and so far, it had a 100% chance of fogging my
brain, making me itch, and dangerously lowering my white count. The doctor
wants me to take this medicine "for the rest of my life, if it works"; I'm
ambivalent, to say the least. Should I feel miserable for 10 months, or feel better
but only have 8 months?
I'm not ready to die, but I don't want to be
sickly. Sometimes I find myself hoping the medicine does not work -- it would
make my decision easier.
I find myself sleeping more, and I'm amazed at
what I used to do! No one would know how sick I am by looking at me help build
the new house, or produce and host my television shows. But I can definitely
tell the difference.
|

|

|
The waiting rooms filled with sick people, the "this won't hurt a bit",
the "the doctor will be right with you" followed by 90 minutes of boredum,
the needle sticks, the smells and taste of medicines, the going home, feeling
sicker and sicker for a week. All of it makes me so tired, I'm sick of it. I've
had enough. If there was hope for a cure, I would say "OK", but they tell me
that the best I can hope for is this, for the rest of my life. If the treatment
"works", I'll live another year, if not, another 9 months. (Those are my guesses).
I'm thinking 9 months may be the way to go . . . I just hope I can be comfortable.
We moved all my stuff into the new house, and are now living with boxes
piled to my shoulders.
I got the news. The chemo is not working. That is,
the dose that allows me to fuction does not prevent tumor growth. So, my choices
are to resume the sickening higher dose, or see if Hopkins has "experimental"
drugs that may help, or say enough is enough. Hopkins is so rude, the chemo
is so noxious, and death is so undesirable, I'm in a no win situation. I'll
talk with the oncologist tomorrow.
|

|
So what does a packrat do with all his stuff he's collected over the years? Example:
I have essentially every significant record released from 1958 to the present. They
grew up with me; they are like family. I had them thru relationships, deaths
in the family, medical school, the ups and downs of life, etc. They might be
worth thousands on the market, but to me, they are priceless. One of my best
friends promises to give them the love and care they deserve, and, over several
weekends, we boxed them up, and he took them to his house, where one of the best
music collections in the world now resides.
|

|


|
I've become very fatigued. When I read the newspaper, I can fall
asleap with ease -- worse than in medical school when they said "first slide,
please". I rest much of the day, and spend the rest of it taking care of the
houses. Packing up the old house allows me to remember the joy my old workbench
gave me. Seeing my Dad's sign reminds me of his inspiration. I knew it was coming!
The oncologist very patiently told me and my family that we've tried essentially
all treatment modalities, and there is little hope. The plan is to keep me as
comfortable as possible, and I hope we are successful.
|
|
|
During this trip thru Hell, I've been impressed with how various
drugs help me -- but imperfectly so -- feel better. Interestingly, although
my physicians are among the world's most knowlegable, even they can't
tell me exactly what drug to take when. I suspect the response to the drugs can be
very idiosyncratic and individual. Click on the button to the right for a listing
of my particular drug experience -- if any one has anything to add, please
write.
|
|
Phrases I now understand (many written on treatment day #43):
- Have a seat, someone will call your name shortly.
- This procedure is very straightforward. Anyone can do it.
- This might hurt a bit.
- After the second week of Cisplatin -- thatís when it gets to them.
- You'll be hungry, but you won't feel like eating.
- If the nausea is intolerable, let us know.
- You might not feel like doing much of anything.
- By the time its time for your surgery, you'll view it as a relief.
- Rejoice in hope, have patience with affliction.
- You'll feel full after you eat even a little.
- Taper off the pain medicine.
- Time may be money, but money can't buy time.
- If you only have a hammer, everything looks like a nail.
- Ultimately, you are alone.
- No one likes a sick person; no one really understands what you are going through.
- Live right, because you may not be able to do it over.
- When a glass is half empty, its also half full.
- Judge a man's character during adversity.
- When you get lemons, make lemonade.
- If you want something done right, you have to do it yourself.
- It is impossible to say "goodbye".
- You have your family, and only a few good friends.
- No one dies wishing they had spent more time in the office.
- Life goes on.
- You are what you do.
- People don't change. If you don't know what is important at 50, you
never will.
|

|
I never thought I would seek so much strength from her, and I don't think
she ever thought she had it in her to give. Click the image at left to see
for yourself! |